Search results (92 results)
-
 Branch Retinal Artery Occlusion
Branch Retinal Artery Occlusion
Dec 19 2025 by Gayathri M S
Multicolor Reflectance and Blue Reflectance of a 55 yr male patient with blurring since 1 month shows classical sectoral retinal whitening.
Photographer: Gayathri MS
Imaging device: Heidelberg Spectralis
Condition/keywords: blue reflectance, branch retinal artery occlusion (BRAO), multicolor
-
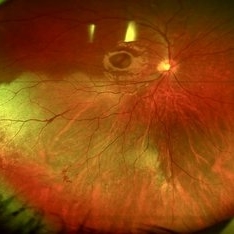
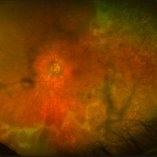
 The Great Vascular Traffic Jam: Combined Retinal Vein and Artery Occlusion
The Great Vascular Traffic Jam: Combined Retinal Vein and Artery Occlusion
Oct 29 2025 by SHRADDHA RAJ SHRIVASTAVA
57 year old female, recently diagnosed with accelerated hypertension, developed Right eye Combined Retinal Vein and Artery Occlusion. Posterior pole image showed severe disc edema with peri-papillary haemorrhages. There is significant retinal whitening suggestive of edema leading to the classic cherry red spot at the macula. We can also see segmented flow of blood in retinal arterioles, which is the characteristic cattle-trucking seen in central retinal artery occlusion (CRAO). Widefield image revealed multiple intra-retinal blot hemorrhages in all quadrants with tortuous dilated vessels suggestive of central retinal vein occlusion (CRVO).
Photographer: Dr. Shraddha Raj Shrivastava
Imaging device: Nidek Mirante SLO/OCT (Confocal scanning/Spectral domain OCT)
Condition/keywords: central retinal vascular obstruction, central retinal vein occlusion (CRVO), CRVO with macular edema
-
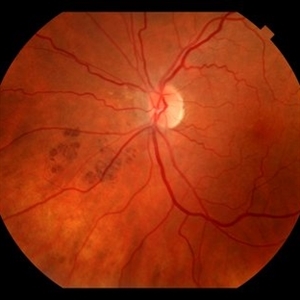
 The Great Vascular Traffic Jam: Combined Retinal Vein and Artery Occlusion
The Great Vascular Traffic Jam: Combined Retinal Vein and Artery Occlusion
Oct 29 2025 by SHRADDHA RAJ SHRIVASTAVA
57 year old female, recently diagnosed with accelerated hypertension, developed Right eye Combined Retinal Vein and Artery Occlusion. Posterior pole image showed severe disc edema with peri-papillary hemorrhages. There is significant retinal whitening suggestive of edema leading to the classic cherry red spot at the macula. We can also see segmented flow of blood in retinal arterioles, which is the characteristic cattle-trucking seen in central retinal artery occlusion (CRAO). Widefield image revealed multiple intra-retinal blot hemorrhages in all quadrants with tortuous dilated vessels suggestive of central retinal vein occlusion (CRVO).
Photographer: Dr. Shraddha Raj Shrivastava
Imaging device: Nidek Mirante SLO/OCT (Confocal scanning/Spectral domain OCT)
Condition/keywords: central retinal artery occlusion (CRAO), central retinal vascular obstruction, central retinal vein occlusion (CRVO), CRVO with macular edema
-
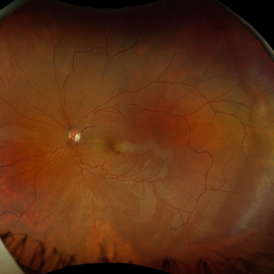
 Central Retinal Artery Occlusion
Central Retinal Artery Occlusion
Sep 30 2025 by César Adrián Gomez Valdivia, MD
This fundus photograph demonstrates the classic retinal whitening due to inner retinal ischemia, with a cherry-red spot at the fovea. The fovea appears red because it is nourished by the intact choroidal circulation, while the surrounding ischemic retina turns pale.
Photographer: @eyemissu2
Imaging device: TOPCON TRX
Condition/keywords: central retinal artery occlusion (CRAO)
-
 Commotio Retinae
Commotio Retinae
Aug 7 2025 by Gabriel Costa Andrade, PhD
Color fundus photograph of a 13-year-old girl who was hit by accidental discharge of gel bullet in her right eye. She presented with retinal whitening with intraretinal hemorrhages in temporal inferior area of the peripheral retina.
Photographer: Gabriel Andrade
Condition/keywords: macula, Retina, Trauma
-
 Patchy Ischemic Whitening in Sturge Weber Syndrome
Patchy Ischemic Whitening in Sturge Weber Syndrome
Nov 18 2024 by Edward F. Hall, MD, FASRS
Left fundus photograph of a 44-year-old man showing patchy ischemic retinal whitening associated with Sturge-Weber Syndrome. The precise cause of this rare complication remains unclear, but it may be linked to choroidal vascular congestion and a compartment syndrome-like effect on the local retinal arteriolar circulation. OCT imaging confirmed inner retinal ischemia and thickening
Photographer: Karissa Kuhl
Imaging device: Optos
Condition/keywords: retinal ischemia, Sturge Weber Syndrome
-
 Cilioretinal Artery Occlusion
Cilioretinal Artery Occlusion
May 14 2024 by Eloy Mata-Cortes, MD
Color image capturing the left eye of a 32-year-old female. Despite a negative ophthalmological and medical history, she reported three days of blurred vision and a paracentral scotoma in her left eye, while maintaining central vision. The image reveals retinal whitening, extends from the parafoveal region to the inferotemporal arcade indicative of cilioretinal artery occlusion. Following this observation, the patient was referred for systemic assessment to explore the underlying etiology of the occlusion.
Photographer: Eloy Mata-Cortes, MD, Instituto Mexicano de Oftalmología, Querétaro, México
Imaging device: Nidek Mirante
Condition/keywords: cilioretinal artery occlusion, oclussion, retinal whitening
-
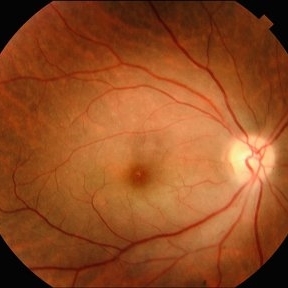
 Central Retinal Artery Occlusion
Central Retinal Artery Occlusion
Nov 16 2023 by Gabriel Costa Andrade, PhD
Fundus photograph of an 62-year-old man with retinal whitening and a cherry red spot due to Central Retinal Artery Occlusion.
Photographer: Gabriel Andrade
Condition/keywords: Central Retinal Artery Occlusion, central retinal artery occlusion (CRAO), Retina
-
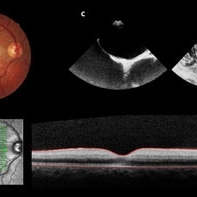
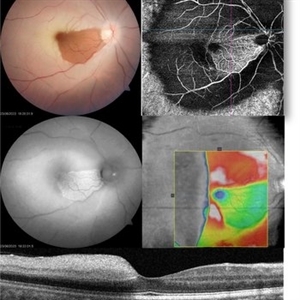 CRAO with cilioretinal sparing - Multimodal imaging
CRAO with cilioretinal sparing - Multimodal imaging
Jun 28 2023 by Maneesh M Bapaye, MD, MBA
A 34 year old male patient presented with sudden onset vision loss of 1 week duration. Visual acuity at presentation was 20/200. Fundus examination revealed diffuse retinal whitening with sparing of papillomacular bundle and fovea due to patent cilioretinal artery. Autofluorescence shows peripheral hypoAF, patent capillaries can be seen only in area of cilioretinal supply, OCT shows thickening of inner retinal layers temporal to fovea Systemic examination revealed that patient had valvular heart disease with multiple valves involved.
Photographer: Maneesh Bapaye
Condition/keywords: cilioretinal sparing, CRAO, multimodal imaging
-
 Commotio-Retinae
Commotio-Retinae
Sep 22 2021 by Luiz Guilherme Freitas, MD, MsC, PhD
Fundus photograph of a 30-year-old male patient with blunt injury to the globe. Commotio retinae is retinal whitening/opacification that results from a blunt injury. The ocular findings will often resolve in a matter of days to weeks. Vision loss can result from commotio involving the posterior pole (historically referred to as Berlin’s edema). Clinical findings of commotio include the characteristic retinal whitening. Commotio may result in significant vision loss that can be transient. Healing can result in pigmentary changes and retinal thinning which may be associated with poor visual recovery if the area of involvement is macular.
Photographer: Diogo Melo, Santa Luzia Eye Hospital Recife - PE – Brazil
Condition/keywords: Berlin's edema, blunt trauma, commotio retinae, retinal whitening
-
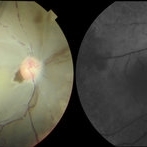
 Acute Central Retinal Artery Occlusion with Natural Reperfusion
Acute Central Retinal Artery Occlusion with Natural Reperfusion
Mar 12 2021 by Kushal S Delhiwala, MBBS, MS, FMRF,FICO, FAICO
Fundus photographs of 33-year-old healthy male with right eye acute CRAO of 12 hours duration showing cattle trucking, extensive retinal whitening and cherry red spot (left image). Right image 18 hours later showing reduced extent of retinal whitening and absent cattle trucking, suggestive of natural restoration of perfusion.
Photographer: Kushal Delhiwala, Netralaya superspeciality eye hospital, Ahmedabad, Gujarat,India
Imaging device: Optos Daytona
Condition/keywords: cattle trucking, central retinal artery occlusion (CRAO), cherry red spot
-
 Central Retinal Artery Occlusion
Central Retinal Artery Occlusion
Jan 22 2021 by Renata Garcia Franco, Md
65-year-old male, history of uncontrolled systemic arterial hypertension. Segmentation of blood in retinal arterioles, retinal whitening and cherry red spot.
Photographer: Fatima Hernandez, Instituto de la Retina del Bajio SC
Imaging device: Zeiss
Condition/keywords: central retinal artery occlusion (CRAO)
-
 Central Retinal Artery Occlusion with Cilioretinal Sparing
Central Retinal Artery Occlusion with Cilioretinal Sparing
Oct 28 2020 by Fang Helen Mi
Fundus photograph of an 61-year-old Chinese male showing central retinal artery occlusion with cilioretinal sparing. Photo shows diffuse ischemic retinal whitening and box-carring of the retinal arterioles.
Condition/keywords: central retinal artery occlusion (CRAO), cilioretinal sparing
-
 Ophthalmic Artery Occlusion in a 39-Year-Old with Rheumatoid Arthritis
Ophthalmic Artery Occlusion in a 39-Year-Old with Rheumatoid Arthritis
Oct 6 2020 by Michael Izzo, MD
Left image: fundus photograph of a 39-year-old male with rheumatoid arthritis found to have ophthalmic artery occlusion depicting boxcar segmentation of blood in retinal vasculature and macular ischemia demonstrated by retinal whitening without cherry red fovea. Right image: early phase fluorescein angiography demonstrating patchy choroidal filling, arterial non-perfusion and optic nerve head leakage.
Photographer: Karen Rivera, COA; Washington National Eye Center
Condition/keywords: fluorescein angiogram (FA), ophthalmic artery occlusion, rheumatoid arthritis
-
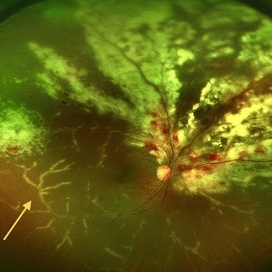 CMV Retinitis with Frosted Branch Angiitis
CMV Retinitis with Frosted Branch Angiitis
Sep 23 2020 by Nimesh A. Patel, MD, FASRS
Fundus photo showing peri-vascular inflammation of both arteries and veins with translucent exudation (yellow arrow). Superior nasally, there is classic retinal whitening with retinal hemorrhages superior. This patient was found to have a low CD4 count and a diagnosis of AIDS was made.
Condition/keywords: cytomegalovirus (CMV), HIV, uveitis
-
 Moyamoya: Photo OD of an Acute CRAO with CRA Sparing
Moyamoya: Photo OD of an Acute CRAO with CRA Sparing
Nov 17 2019 by John S. King, MD
60-year-old white female presented with five days of acute vision loss in the right eye. She was seen initially by referring doctor after hours five days ago and diagnosed with a CRAO and sent to ED to be evaluated stroke team. Right ICA was 100% closed but completely bypassed. She called four days later c/o redness and eye pain; at this point prominent iris vessels were seen, and she was sent to us. Her background history includes a diagnosis of moyamoya (underwent bilateral cerebral artery bypass 2015); atorvastatin for hypercholesterolemia; ASA; no hx of HTN or heart disease. She had a scleral buckle repair OD in 2017 and later developed a thick ERM, which was repaired in 2018; on her previous visit her acuity was noted at 20/40. On presentation her visual acuity was HM OD and 20/15 OS. IOP was 8 OD and 10 OS. There were prominent iris vessels in the right eye, no cell or flare, and an IOL. The posterior segment exam showed diffuse retinal whitening with attenuated vessels and boxcarring; there was sparing retinal whitening in a central area of the macula that appeared to be supplied by a cilio-retina artery. The FA showed very slow filling of the retinal vessels; there was some early perfusion secondary to the cilio-retinal artery. At 7 minutes there was still significant areas of non-perfusion, as well as macular ischemia. Avastin was administered, and one week later, PRP was performed. On the day PRP was performed, the irregular iris vessels had regressed completely. She said that she had a "sliver" of vision centrally in that eye; her acuity was CF 2' and IOP 12.
Photographer: Gretchen Harper
Imaging device: Topcon
Condition/keywords: central retinal artery occlusion (CRAO), cilioretinal sparing, moyamoya, neovascularization of iris (NVI)
-
 Moyamoya: FA 52 Sec OD of an Acute CRAO with CRA Sparing
Moyamoya: FA 52 Sec OD of an Acute CRAO with CRA Sparing
Nov 17 2019 by John S. King, MD
60-year-old white female presented with five days of acute vision loss in the right eye. She was seen initially by referring doctor after hours five days ago and diagnosed with a CRAO and sent to ED to be evaluated stroke team. Right ICA was 100% closed but completely bypassed. She called four days later c/o redness and eye pain; at this point prominent iris vessels were seen, and she was sent to us. Her background history includes a diagnosis of moyamoya (underwent bilateral cerebral artery bypass 2015); atorvastatin for hypercholesterolemia; ASA; no hx of HTN or heart disease. She had a scleral buckle repair OD in 2017 and later developed a thick ERM, which was repaired in 2018; on her previous visit her acuity was noted at 20/40. On presentation her visual acuity was HM OD and 20/15 OS. IOP was 8 OD and 10 OS. There were prominent iris vessels in the right eye, no cell or flare, and an IOL. The posterior segment exam showed diffuse retinal whitening with attenuated vessels and boxcarring; there was sparing retinal whitening in a central area of the macula that appeared to be supplied by a cilio-retina artery. The FA showed very slow filling of the retinal vessels; there was some early perfusion secondary to the cilio-retinal artery. At 7 minutes there was still significant areas of non-perfusion, as well as macular ischemia. Avastin was administered, and one week later, PRP was performed. On the day PRP was performed, the irregular iris vessels had regressed completely. She said that she had a "sliver" of vision centrally in that eye; her acuity was CF 2' and IOP 12.
Photographer: Gretchen Harper
Imaging device: Topcon
Condition/keywords: central retinal artery occlusion (CRAO), cilioretinal sparing, moyamoya, neovascularization of iris (NVI)
-
 Moyamoya: FA 2 Min OD of an Acute CRAO with CRA Sparing
Moyamoya: FA 2 Min OD of an Acute CRAO with CRA Sparing
Nov 17 2019 by John S. King, MD
60-year-old white female presented with five days of acute vision loss in the right eye. She was seen initially by referring doctor after hours five days ago and diagnosed with a CRAO and sent to ED to be evaluated stroke team. Right ICA was 100% closed but completely bypassed. She called four days later c/o redness and eye pain; at this point prominent iris vessels were seen, and she was sent to us. Her background history includes a diagnosis of moyamoya (underwent bilateral cerebral artery bypass 2015); atorvastatin for hypercholesterolemia; ASA; no hx of HTN or heart disease. She had a scleral buckle repair OD in 2017 and later developed a thick ERM, which was repaired in 2018; on her previous visit her acuity was noted at 20/40. On presentation her visual acuity was HM OD and 20/15 OS. IOP was 8 OD and 10 OS. There were prominent iris vessels in the right eye, no cell or flare, and an IOL. The posterior segment exam showed diffuse retinal whitening with attenuated vessels and boxcarring; there was sparing retinal whitening in a central area of the macula that appeared to be supplied by a cilio-retina artery. The FA showed very slow filling of the retinal vessels; there was some early perfusion secondary to the cilio-retinal artery. At 7 minutes there was still significant areas of non-perfusion, as well as macular ischemia. Avastin was administered, and one week later, PRP was performed. On the day PRP was performed, the irregular iris vessels had regressed completely. She said that she had a "sliver" of vision centrally in that eye; her acuity was CF 2' and IOP 12.
Photographer: Gretchen Harper
Imaging device: Topcon
Condition/keywords: central retinal artery occlusion (CRAO), cilioretinal sparing, moyamoya, neovascularization of iris (NVI)
-
 Moyamoya: FA 3:25 OD of an Acute CRAO with CRA Sparing
Moyamoya: FA 3:25 OD of an Acute CRAO with CRA Sparing
Nov 17 2019 by John S. King, MD
60-year-old white female presented with five days of acute vision loss in the right eye. She was seen initially by referring doctor after hours five days ago and diagnosed with a CRAO and sent to ED to be evaluated stroke team. Right ICA was 100% closed but completely bypassed. She called four days later c/o redness and eye pain; at this point prominent iris vessels were seen, and she was sent to us. Her background history includes a diagnosis of Moyamoya (underwent bilateral cerebral artery bypass 2015); atorvastatin for hypercholesterolemia; ASA; no hx of HTN or heart disease. She had a scleral buckle repair OD in 2017 and later developed a thick ERM, which was repaired in 2018; on her previous visit her acuity was noted at 20/40. On presentation her visual acuity was HM OD and 20/15 OS. IOP was 8 OD and 10 OS. There were prominent iris vessels in the right eye, no cell or flare, and an IOL. The posterior segment exam showed diffuse retinal whitening with attenuated vessels and boxcarring; there was sparing retinal whitening in a central area of the macula that appeared to be supplied by a cilio-retina artery. The FA showed very slow filling of the retinal vessels; there was some early perfusion secondary to the cilio-retinal artery. At 7 minutes there was still significant areas of non-perfusion, as well as macular ischemia. Avastin was administered, and one week later, PRP was performed. On the day PRP was performed, the irregular iris vessels had regressed completely. She said that she had a "sliver" of vision centrally in that eye; her acuity was CF 2' and IOP 12.
Photographer: Gretchen Harper
Imaging device: Topcon
Condition/keywords: central retinal artery occlusion (CRAO), cilioretinal sparing, moyamoya, neovascularization of iris (NVI)
-
 Moyamoya: FA 7 Min OD of an Acute CRAO with CRA Sparing
Moyamoya: FA 7 Min OD of an Acute CRAO with CRA Sparing
Nov 17 2019 by John S. King, MD
60-year-old white female presented with five days of acute vision loss in the right eye. She was seen initially by referring doctor after hours five days ago and diagnosed with a CRAO and sent to ED to be evaluated stroke team. Right ICA was 100% closed but completely bypassed. She called four days later c/o redness and eye pain; at this point prominent iris vessels were seen, and she was sent to us. Her background history includes a diagnosis of Moyamoya (underwent bilateral cerebral artery bypass 2015); atorvastatin for hypercholesterolemia; ASA; no hx of HTN or Heart Disease. She had a scleral buckle repair OD in 2017 and later developed a thick ERM, which was repaired in 2018; on her previous visit her acuity was noted at 20/40. On presentation her visual acuity was HM OD and 20/15 OS. IOP was 8 OD and 10 OS. There were prominent iris vessels in the right eye, no cell or flare, and an IOL. The posterior segment exam showed diffuse retinal whitening with attenuated vessels and boxcarring; there was sparing retinal whitening in a central area of the macula that appeared to be supplied by a cilio-retina artery. The FA showed very slow filling of the retinal vessels; there was some early perfusion secondary to the cilio-retinal artery. At 7 minutes there was still significant areas of non-perfusion, as well as macular ischemia. Avastin was administered, and one week later, PRP was performed. On the day PRP was performed, the irregular iris vessels had regressed completely. She said that she had a "sliver" of vision centrally in that eye; her acuity was CF 2' and IOP 12.
Photographer: Gretchen Harper
Imaging device: Topcon
Condition/keywords: central retinal artery occlusion (CRAO), cilioretinal sparing, moyamoya, neovascularization of iris (NVI)
-
 Progressive Outer Retinal Necrosis
Progressive Outer Retinal Necrosis
Nov 5 2019 by Nichole Lewis
86-year-old male with progressive outer retinal necrosis, significant retinitis, retinal whitening, intraretinal hemorrhages and peripheral rpe changes. FA showed occlusive vasculitis with non-perfusion. Patient is immuno-suppressed with a history of renal transplant. VA 20/60.
Photographer: Nichole Lewis
Imaging device: Optos
Condition/keywords: intraretinal hemorrhage, occlusive vasculitis, progressive outer retinal necrosis (PORN), retinal pigment epithelium (RPE) changes, retinal whitening, retinitis
-
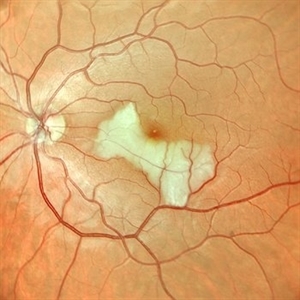
 Central Retinal Artery Occlusion Leading to Patent Foramen Ovale Diagnosis
Central Retinal Artery Occlusion Leading to Patent Foramen Ovale Diagnosis
Sep 13 2019 by Patrícia José Figueiredo Lopes
A 19-year-old man presented in emergency department (ED) reporting painless blurred vision in the right eye that started one hour ago while he was doing exercise. His medical history was unremarkable. On examination, best corrected visual acuity in the right eye was counting fingers (20cm), right relative afferent pupillary defect was evident, intraocular pressure and anterior segment were normal. Dilated retinal examination revealed retinal whitening in the macular area and a cherry red spot (panel A) that became increasingly evident with time. Patient denied other systemic symptoms. Macular spectral domain optic coherence tomography showed hyperreflectivity of the inner retina (panel B). In ED, patient underwent ocular massage using a three-mirror contact lens and topical hypotensive treatment. Additionally, oral antiplatelet and hyperbaric oxygen treatment were initiated. Further investigation was performed and fluorescein angiography revealed a delay in arterial filling. Blood tests including hypercoagulation disorders investigation, plain chest radiography and electrocardiogram were unremarkable. Patent foramen ovale was diagnosed in transesophageal echocardiogram (panel C), anticoagulation therapy was promptly initiated and percutaneous closure of patent foramen ovale was done successfully a few weeks later. Final best corrected visual acuity was 20/200 and macula developed atrophy.
Photographer: Patrícia José
Condition/keywords: central retinal artery occlusion (CRAO), patent foramen ovale
-
 Acute Compressive Optic Neuropathy
Acute Compressive Optic Neuropathy
Jun 1 2019 by John S. King, MD
84-year-old white female with acute loss of vision in the left eye one day ago was sent here after going to the ED per primary eye provider. She described vision loss as a grey curtain that became total darkness. She had left sided temporal tenderness and some left sided neck pain. In the ED the cardiac work-up was u/r, the ESR and CRP were normal, and the CTH showed some non-specific opacification in the L ethmoid sinus. Acuity was HM OS with RAPD, normal EOMs, no proptosis or ptosis, posteriorly no SVPs were noted; the optic discs were pink and flat; no emboli or retinal whitening present; some bear tracks located nasally (see photo). She was referred to Dr. Doyle, who ordered an MRI, which showed a large mucocele with bony erosion into the left orbit, along with some ON enhancement possibly from compression (see images). She was operated that night and later recovered to 20/40 in that eye with a residual, inferior arcuate scotoma.
Condition/keywords: bear tracks, optic neuropathy
-
 Acute Optic Neuropathy Due to Large Mucocele
Acute Optic Neuropathy Due to Large Mucocele
Jun 1 2019 by John S. King, MD
84-year-old white female with acute loss of vision in the left eye one day ago was sent here after going to the ED per primary eye provider. She described vision loss as a grey curtain that became total darkness. She had left sided temporal tenderness and some left sided neck pain. In the ED the cardiac work-up was u/r, the ESR and CRP were normal, and the CTH showed some non-specific opacification in the L ethmoid sinus. Acuity was HM OS with RAPD, normal EOMs, no proptosis or ptosis, posteriorly no SVPs were noted; the optic discs were pink and flat; no emboli or retinal whitening present; some bear tracks located nasally (see photo). She was referred to Dr. Doyle, who ordered an MRI, which showed a large mucocele with bony erosion into the left orbit, along with some ON enhancement possibly from compression (see Images). She was operated that night and later recovered to 20/40 in that eye with a residual, inferior arcuate scotoma.
Condition/keywords: bear tracks, optic neuropathy
-
 Acute Optic Neuropathy Due to Large Mucocele (Incidental Bear Tracks)
Acute Optic Neuropathy Due to Large Mucocele (Incidental Bear Tracks)
Jun 1 2019 by John S. King, MD
84-year-old white female with acute loss of vision in the left eye one day ago was sent here after going to the ED per primary eye provider. She described vision loss as a grey curtain that became total darkness. She had left sided temporal tenderness and some left sided neck pain. In the ED the cardiac work-up was u/r, the ESR and CRP were normal, and the CTH showed some non-specific opacification in the L ethmoid sinus. Acuity was HM OS with RAPD, normal EOMs, no proptosis or ptosis, posteriorly no SVPs were noted; the optic discs were pink and flat; no emboli or retinal whitening present; some bear tracks located nasally (see photo). She was referred to Dr. Doyle, who ordered an MRI, which showed a large mucocele with bony erosion into the left orbit, along with some ON enhancement possibly from compression (see images). She was operated that night and later recovered to 20/40 in that eye with a residual, inferior arcuate scotoma.
Photographer: Karin Aletter
Imaging device: Topcon 50
Condition/keywords: bear tracks, optic neuropathy

 Loading…
Loading…