-
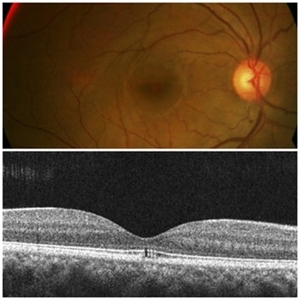
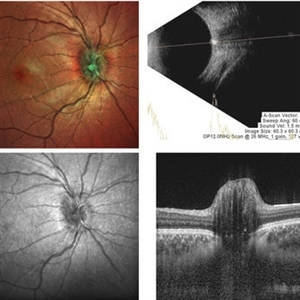 ONH-Drusen
ONH-Drusen
-
 ONH-Drusen
ONH-Drusen
-
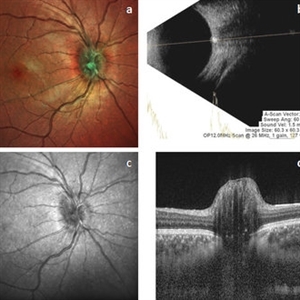
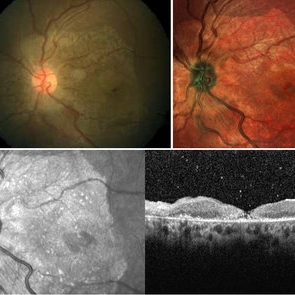
 Outer Retinal Tubulation
Outer Retinal Tubulation
Mar 27 2018 by Dhaivat Shah
Outer retinal tubulation (ORT) is a feature of photoreceptor rearrangement after chronic retinal damage due to refractory cme, long standing CNVM or old trauma. Photoreceptors lose adhesions to surrounding structures, resulting in outward folding and formation of new lateral contact between photoreceptors to form round structure. They generally remains stable over time. It is important to recognize ORT on OCT because it indicates a refractory state of the pathological condition and poor visual prognosis, and likely not to benefit from any treatment. Here is a case of 62-year-old female with history of 4 previous anti-VEGF injection in left eye for CNVM, with the recent OCT showing formation of ORT with subfoveal scarred membrane.
Photographer: Dr Dhaivat Shah
Condition/keywords: choroidal neovascular membrane (CNVM), outer retinal tubulation
-
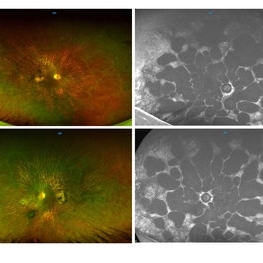
 Cystoid Macular Edema Multicolor imaging
Cystoid Macular Edema Multicolor imaging
Mar 31 2018 by Dhaivat Shah
This is a case of a 50-year-old female presenting with right eye IT BRVO with ME. Unarguably, the first modality of investigation would be an OCT along with a fundus photograph. Instead of using a conventional fundus photo, a multicolor image was captured. It beautifully highlighted the cystic pattern of macular edema, hemorrhages and sclerosed vessel, which corresponded well with the OCT findings. Multi-color scanning laser imaging uses three laser wavelengths simultaneously to provide diagnostic images that show distinct structures at different depths within the retina. The high-resolution, detailed MultiColor images can highlight structures and pathologies not visible on ophthalmoscopy and fundus photography. This imaging modality has the potential to replace conventional color fundus photography in the near future.
Photographer: Dr Dhaivat Shah
Imaging device: Heidelberg Spectralis
Condition/keywords: cystoid macular edema (CME), multicolor
-
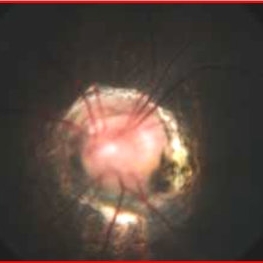 Morning Glory Syndrome
Morning Glory Syndrome
Apr 14 2018 by Dhaivat Shah
7-year-old male patient presented to our OPD when the mother noticed that the child is not able to see clearly through the left eye. BCVA OD 6/6 OS 6/60. OU anterior segment normal. Fundus OD was normal, OS showed an enlarged, funnel-shaped excavation that incorporated the optic disc. The disc itself was enlarged, pink in color and had a surrounding area of peripapillary chorioretinal pigmentary changes which was sparing the fovea. MRI orbit/brain came out to be normal. OS diagnosed to be Morning glory syndrome. The child was prescribed full-time glasses to correct the anisometropia and occlusion/patching of the right(normal) eye 2 hours per day and guarded visual prognosis was explained.
Photographer: Miss Marina Parvin
Condition/keywords: Morning Glory Syndrome
-
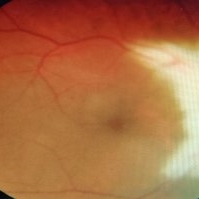
 Foveal Thinning Post Blunt Trauma
Foveal Thinning Post Blunt Trauma
Aug 25 2018 by Dhaivat Shah
28-year-old male. Post blunt trauma with tennis ball. Fundus color photo shows large area of retinal thinning. Multi color image shows dull red color over fovea, depicting thinning. SD-OCT shows inner retinal ischemia and foveal thinning with early macular hole formation.
Imaging device: Spectralis
Condition/keywords: blunt trauma
-
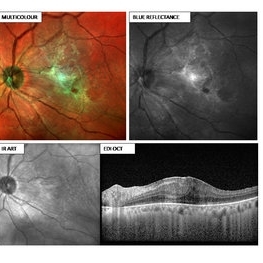 ERM
ERM
Aug 30 2018 by Dhaivat Shah
55-year-old female presented with left eye BCVA 6/24 N18, early cataract changes on slit lamp, fundus showing ERM with retinal thickening. Multi-color image (MCI) depicting an ERM (green hue) with retinal thickening. Note how beautifully the extent of ERM is captured, which can help the surgeon to decide the area of surgical peeling. The BR particularly provides details of the inner retina and the vitreoretinal interface, hence showing the ERM. This platform utilizes confocal technology and thus has unique advantages over CFP. MCI provides good image quality in hazy media and in small pupil. It does not use bright white light and thus is not discomforting to the patient. Images obtained with MCI have better contrast and sharper borders as compared to CFP. Definitely the new tech in for the next generation!
Photographer: Miss Moupiya Das
Imaging device: SPECTRALIS
Condition/keywords: blue reflectance, epiretinal membrane (ERM)
-
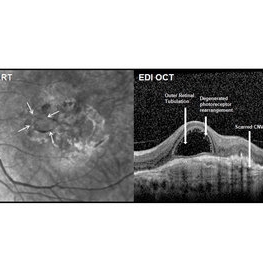
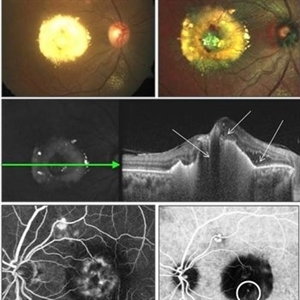 Polypoidal Chroidal Vasculopathy
Polypoidal Chroidal Vasculopathy
Sep 21 2018 by Dhaivat Shah
A 40-year-old female presented with sudden onset decreased vision in right eye. BCVA: CF 1 mt. Fundus showed massive subretinal exudation with haemorrhage. EDI OCT showed notched PEDs with shallow SRF and exudation with back-shadowing. FFA shows leak with window defects. ICG shows hotspot in late phase. Polypoidal choroidal vasculopathy (PCV) is a retinal disorder characterized by the presence of aneurysmal polypoidal lesions in the choroidal vasculature, resulting in damage to the overlying retina and loss of retinal pigment epithelium. The aneurysmal dilatations, also known as polyps, may be found subfoveal, juxtafoveal, extrafoveal, peripapillary or even peripheral regions. The polypoidal lesions are best detected on indocyanine green angiography as hotspots in late phase. The presence of choroidal polyps can lead to recurrent episodes of exudative retinal detachment, serous or hemorrhagic pigment epithelial detachment, subretinal hemorrhage and exudation. Treatment is available in form of laser/PDT along with Anti VEGF injection.
Photographer: Miss Moupiya Das
Condition/keywords: polypoidal choroidal vasculopathy (PCV)
-
 Gyrate Atrophy
Gyrate Atrophy
Oct 31 2018 by Dhaivat Shah
50-year-old male came in with complaint of daytime vision loss for a year and nighttime vision loss for more than 20 years, gradually increasing day by day. Fundus showed paving-stone like areas of atrophy of the RPE involving the macula which coalesces to form a characteristic scalloped border at the junction of normal and abnormal RPE. Gyrate atrophy is an autosomal recessive dystrophy caused by tenfold elevations of plasma ornithine, which is toxic to the RPE and choroid. Patients with gyrate atrophy have hyperpigmented fundi, with lobular loss of the RPE and choroid, normally sparing the fovea. The finding of generalized hyperpigmentation of the remaining RPE helps to clinically distinguish gyrate atrophy from choroideremia. Affected patients usually develop night blindness during the first decade of life and experience progressive loss of visual field and visual acuity later in the disease course. Early diagnosis is crucial because treatment in form of Arginine free diet and oral pyridoxine helps in slowing the progression of disease.
Imaging device: Optos
Condition/keywords: fundus autofluorescence (FAF), gyrate atrophy
-
 Peri-papillary Vascular Loop
Peri-papillary Vascular Loop
Jun 2 2020 by Dhaivat Shah
Peri-papillary vascular loops (PVL) are rare congenital vascular malformations, which are usually detected as accidental finding during routine fundus examination. They can often be confused with tributary vein occlusion or racemose hemangioma. Although benign and asymptomatic, they can be rarely associated with vitreous hemorrhage and arterial occlusion. We herein present a case of a 60-year-old hypertensive male, who was diagnosed elsewhere to have a tributary vein occlusion and was referred to us. FFA was advised to rule out neovascularization, surrounding capillary non perfusion and mass lesion (hemangioma). On FFA, the arterial loop showed a slightly delayed filling (3-5 seconds) as compared to the other arterial vessels and the original vessel appeared to be a branch arising from central retinal artery. The choroidal filling was delayed in the area supplied by the loop. A cilioretinal artery was also noted. The patient was diagnosed to have a Peri-papillary vascular arterial loop (PVL), likely to be congenital in origin. The patient was reassured and was advised yearly follow up. These loops are usually accidental findings discovered during routine fundus examination. Since these vessels are looped and tortuous, they exhibit a slower and laminar blood flow, which make them more prone for arterial occlusions. The vitreous in this area tends to be adherently attached, so during PVD induction, it is likely to cause a tear and hemorrhage leading to vitreous hemorrhage. Until and unless there is a break, this hemorrhage tends to resolve on its own and does not warrant treatment. If there is an evident break, it can be dealt with laser barrage.
Photographer: Choithram Netralaya
Condition/keywords: congenital prepapillary vascular loop
-
 Myelinated Nerve Fiber (mNFL)
Myelinated Nerve Fiber (mNFL)
Jun 21 2020 by Dhaivat Shah
Myelinated nerve fiber layer (mNFL) is a benign clinical entity that results from an embryologic developmental anomaly. Myelination along the visual pathway is noted around the eighth month of gestation, and typically reaches the posterior globe around the time of birth with virtually all fibers reaching complete myelination by age 7 months till the lamina cribrosa. Sometimes, due to altered neuro hormonal signals, this process of myelination extends past the lamina cribrosa and is visible on fundus examination as distinct white patches on the inner retinal surface. On infrared and red-free imaging, mNFL appears white, which is likely due to the high lipid content of myelin. Myelin blocks detection of underlying fluorescent material, thus appearing dark on fundus autofluorescence. On optical coherence tomography , it appears as a thickened and hyperreflective retinal nerve fiber layer. mNFL is typically benign but can be mistaken for other potentially serious conditions like neoplastic infiltration or infection. Hence, it is crucial to recognize the benign nature of mNFL to avoid superfluous medical testing.
Photographer: Ms Srishti Sharma
Imaging device: Choithram Netralaya
Condition/keywords: myelinated nerve fibers
-
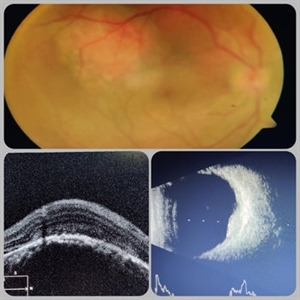 Circumscribed Choroidal Hemangioma
Circumscribed Choroidal Hemangioma
Jul 3 2020 by Dhaivat Shah
A 30-year-old young male presented with drop in vision in right eye since 1 year (6/60). Fundus examination revealed choroidal hemangioma superotemporal to macula. Choroidal hemangioma is an unusual benign vascular tumor of the choroid. It can be circumscribed solitary or diffuse tumor with the later having other systemic associations. Circumscribed choroidal hemangiomas (CCHs) are usually unilateral, unifocal hamartomatous vascular tumor affecting people in second to fourth decade. It appers as round to oval, orangish-red mass in posterior pole with smooth homogenous surface mostly present in macular and peripapillary area. Hyperopic shift is seen in sub-foveal tumors in contrast to para-foveal ones which are usually asymptomatic or present with metamorphopsia or photopsia and diminished vision secondary to exudative retinal detachment. B-scan shows highly reflective tumor without any shadowing or acoustic solidity with high anterior A scan spike. EDI-OCT here depicts a smooth gently sloping choridal mass with compressed choriocapillaries and enlarged medium and large choroidal vessels. Over a period of time structural abnormalities of the outer retina can be visualised. Ancillary testing using Fluorescein Angiography shows lacy hyper-fluorescence during early arterial phase followed by increased hyper-fluorescence due to progressive profuse leakage from pin point foci during arterial and venous phase. Indocyanine green angiography shows lacy diffuse fluorescent tumor in early phase followed by hypo-fluorescent tumor due to dye wash out in late phase. Intrinsic auto-fluorescence is also seen in CCHs from lipofuscin and fresh sub-retinal fluid. Tumor is relatively hyper-intense with respect to vitreous in T1-weighted images in iso-intense in T2-weighted images of MRI. Asymptomatic cases need no treatment, while patients showing vision loss with presence or absence of exudative retinal detachment can be treated with photodynamic therapy which is preferred treatment due to site specific action. Selective occlusion of choroidal neovascularization can be achieved while the neurosensory retinal layers and Bruch membrane are almost unaffected, leaving retinal function intact. Green or rarely red wavelength laser photocoagulation is used to create a chorioretinal adhesion and resolve the SRF. Other treatment modalities include Transpupilary thermotherapy, external beam irradiation, proton beam therapy, brachytherapy and gamma knife.
Photographer: Miss Deepika Nagle
Imaging device: Zeiss
Condition/keywords: B scan ultrasound, choroidal hemangioma, fundus photograph, optical coherence tomography (OCT), photodynamic therapy
-
cRORA
Aug 5 2020 by Dhaivat Shah
A 54-year-old healthy male presented to us with a decreased vision in right eye since past 8 years. The patient gave a history of bleed in right eye before 8 years for which some intravitreal injection was given; post which there no major visual improvement. No details or documentation was available regarding the same. His BCVA in the right eye was 5/60. Fundus examination revealed a sharply demarcated hypopigmented patch over the macula with mild posterior excavation suggestive of macular scar. OCT image shows foveal thinning with loss of Retinal pigment epithelium and outer retinal layers (RORA). There are 2 types of RORAs, complete and incomplete. Complete RORA and incomplete RORA are entities defined by various imaging modalities describing atrophy of the retinal pigment epithelial and the outer retinal layers. OCT imaging defines incomplete RORA (iRORA) as a region of signal hyper transmission into the choroid and a corresponding zone of attenuation ordisruption of the RPE (<250um) and evidence of overlying photoreceptor degeneration (<250um). There should not be any RPE tear associated with it. OCT imaging describes complete RORA (cRORA) based on 4 inclusion criteria. These include, area of hypertransmission of more than 250um, zone of attenuation or disruption of the RPE of more than 250um in diameter, evidence of overlying photoreceptor degeneration and absence of scrolled RPE or other signs of an RPE tear. Other modalities used to define these include fundus autoflourescence(FAF), near infrared reflectance(NIR) and color fundus photograph(CFP). On CFP, it shows a sharply demarcated hypopigmented of >250um size with better visibility of choroidal vessels. FAF shows a hypo autoflourescent patch with sharply demarcated borders of size >250um, the colour of which is similar to that of the optic nerve head or retinal blood vessels excluding any pigmentation or artefact. On NIR, it shows a hyperreflective area with sharply demarcated borders of >250um size excluding any artefact. RORA can be seen in conditions like geographical atrophy in ARMD, central areolar choroidal dystrophy, atrophy secondary to anti-VEGF treatment. References: 1. Sadda SR, Guymer R, Holz FG, et al. Consensus Definition for Atrophy Associated with Age-Related Macular Degeneration on OCT: Classification of Atrophy Report 3 [published correction appears in Ophthalmology. 2019 Jan;126(1):177]. Ophthalmology. 2018;125(4):537-548. 2. Guymer RH, Rosenfeld PJ, Curcio CA, et al. Incomplete Retinal Pigment Epithelial and Outer Retinal Atrophy in Age-Related Macular Degeneration: Classification of Atrophy Meeting Report 4. Ophthalmology. 2020;127(3):394-409. 3. Eng VA, Rayess N, Nguyen HV, Leng T. Complete RPE and outer retinal atrophy in patients receiving anti-VEGF treatment for neovascular age-related macular degeneration. PLoS One. 2020;15(5):e0232353.
Photographer: Miss Anjum Zafar Khan
Imaging device: Choithram Netralaya
Condition/keywords: macular scar, outer retina, retinal pigment epithelium
-
Bergmeister's Papilla
Sep 29 2020 by Dhaivat Shah
Bergmeister's papilla is a small tuft of glial tissue which arises from the center of the optic disc, and represents a remnant of the fetal hyaloid artery. The hyaloid artery provides nutrition to the lens during development, and runs forward to the lens from the optic disc. At birth the hyaloid artery regresses, and is normally completely regressed by the time of birth. Bergmeister's papilla is frequently observed as an incidental clinical finding if this artery has an incomplete regression posteriorly. However, in the severe forms it can be associated with cataracts, persistence of the primitive vitreous, microphthalmia, vitreous hemorrhages and sometimes tractional retinal detachment, due to contraction of the residual fibro vascular tissue. Therefore, careful monitoring of vitreous thickening in the peripapillary areas, both by examining the ocular fundus, and especially by SD-OCT, is of considerable importance. Here we have one such of a 30 year old young male who came in for a routine checkup, in whom we noted a Bergmeister’s papilla. Due to its benign nature, patient was reassured and was asked to follow up yearly.
Condition/keywords: Bergmeister's Papillae
-
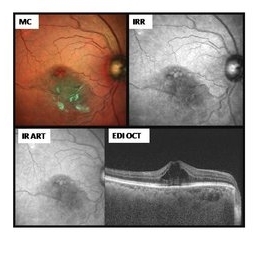
 Retinal Angiomatous Proliferation
Retinal Angiomatous Proliferation
May 7 2021 by Dhaivat Shah
Retinal angiomatous proliferation (RAP) is a distinct variant of neovascular age-related degeneration (AMD) that usually initiates at the retina and progresses posteriorly into sub retinal space. In most recent study, it was suggested that angiogenesis may begin in the retina, choroid, or both, and introduced a new name for the process: Type 3 neovascularization. The frequency of RAP has been studied in many studies, with figures ranging from 10% to 21% of exudative AMD. Clinically, three stages were originally described as intraretinal neovascularization (IRN), subretinal neovascularization (SRN), choroidal neovascularization (CNV). RAP predominantly intraretinal hard exudates, and intra/pre retinal hemorrhages along with intraretinal edema, associated pigment epithelial detachment beneath it, at times retinochoroidal, retino-retinal anastomosis. Apart from conventional OCT, FFA and ICG, OCT-A has now been used primarily as a tool in the diagnosis RAP. Here we present imaging of a 30-year-old young male diagnosed as RAP stage 3 (Type 3 CNVM). Patient was started on intravitreal anti-VEGF monotherapy therapy.
Photographer: Choithram Netralaya Indore
Condition/keywords: retinal angiomatous proliferation (RAP)
-
 Arc Welder's Maculopathy
Arc Welder's Maculopathy
Jun 2 2021 by Dhaivat Shah
Unlike arc-welding induced photokeratoconjuctivitis i.e. ‘arc’s eye’ known to most of the clinicians, macular injury is unusual to happen. It is a rare type of photic or UV retinopathy caused by exposure to electric arc welding light which emits wide spectrum of radiations ranging from UV to infrareds through penetrating into the retina. A 35-year-old male, a professional welder, presented with mild blurring of vision in both eyes. Fundus revealed dull foveal reflex (OU) with subtle foveal alterations surrounded by halo (right more prominent than left eye). He later revealed a history of infrequent use of protective glasses during work. OCT is a very sensitive test to establish diagnosis, which ellipsoid zone disturbance as a square shaped defect, keeping the RPE & ELM intact. Patient was explained guarded visual prognosis and was advised strictly to wear protective eye gears at work.
Photographer: Choithram Netralaya
Imaging device: Zeiss
Condition/keywords: Welding arc maculopathy
-
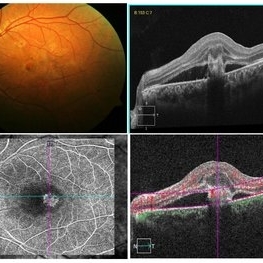
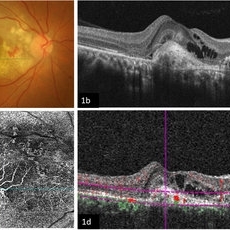 Imaging Feeder Vessels on OCT-A in a case of Retinal Angiomatous Proliferation
Imaging Feeder Vessels on OCT-A in a case of Retinal Angiomatous Proliferation
Feb 24 2023 by Dhaivat Shah
A 58-year-old male patient, a chronic smoker, came to our OPD with complaints of a diminution of vision in the right eye (BCVA: 2/60). On examination, the following findings were observed in the patient. On fundus examination (Image 1a) - Large areas of exudation with multiple superficial and deep hemorrhages at the macula were noted. On SD-OCT imaging (Image 1b) - Multiple intraretinal spaces were seen along with shallow subretinal fluid and hyperreflective dots (indicative of phagocytosed photoreceptors). On the foveal area- a hyperreflective membrane was noted which seemed to dip down and establish a retino-choroidal anastomosis. On OCT-A imaging (Image 1c) - In the ORCC complex, the neovascularization frown, correlating with the membrane complex on the fundus and structural OCT, was visible which was noted to be supplied by small feeder vessels coming from the superior aspect of the fovea. On OCT-A blood flow analysis imaging (Image 1d) - The blood flow analysis showed increased blood flow signals at the level of the membrane (indicative of increased color signal). Based on the findings of the above investigations and clinical examination, the patient was diagnosed with a Case of CNVM Type 3, also described as RAP, and was managed by Anti VEGF injections. This condition usually requires more injections as compared to Type 1 and 2 CNVMs, and the visual prognosis is guarded. Hence, it's very important to counsel the patient before initiating the treatment that the treatment would be long-term and the aim would be preservation of existing vision.
Photographer: Choithram Netralaya, Indore
Condition/keywords: feeder vessel, OCTA, RAP lesion

A project from the American Society of Retina Specialists