Search results (1033 results)
-
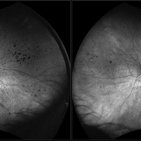
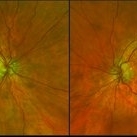
 Bilateral Calcific Retina Arteriolar Occlusions in a Patient with Metastatic Ovarian Carcinoma
Bilateral Calcific Retina Arteriolar Occlusions in a Patient with Metastatic Ovarian Carcinoma
Dec 10 2020 by McGill University Health Centre
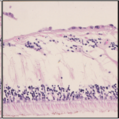
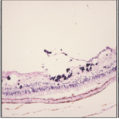
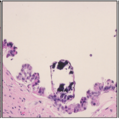
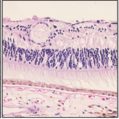
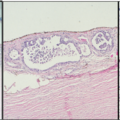
47-year-old female with cough and fever. Imaging showed a right pulmonary infiltrate. Transbronchial needle biopsy revealed lymphangitic spread of papillary adenocarcinoma with psammoma bodies (MRI of thyroid, CT of abdomen and pelvis were negative) gynecologic evaluation negative at that time . The patient had bilateral floaters, VA: 20/40 OD and 20/20 OS. Fundus examination showed retinal arteriolar sheathing and a flat choroidal lesion OS and vitritis OD. Fluorescein angiogram showed staining of left superior temporal retinal arterioles and bilateral midperipheral patchy hyperfluorescence at RPE. The patient vision in the OD deteriorated to 20/400, and in the OS 20/50. Four months later a new choroidal lesion was diagnosed OS. An abdominal mass consistent with a cystadenoma of the ovary was diagnosed. After a year patient developed systemic metastasis. Autopsy: Metastatic adenocarcinoma to the lung, both adrenals, para-aortic lymph nodes, left hip, right breast, occipital skin, serosal surface of liver, pituitary. In almost all metastatic lesions psammoma bodies were found. Presumptive diagnosis is a primary tumor of the ovary. Histopathologic examination of both eyes disclosed : Bilateral metastatic adenocarcinoma to the vitreous with partially calcified proliferation along internal limiting membrane, OS. Metastatic adenocarcinoma to choroid, OS. Bilateral optic atrophy secondary to retinal arteriolar occlusion with calcification.
Condition/keywords: bilateral, calcification, histopathology, metastatic adenocarcinoma, pathology, retinal arteriolar occlusion
-
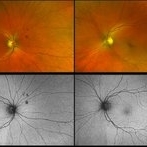
 Bilateral Calcific Retina Arteriolar Occlusions in a Patient with Metastatic Ovarian Carcinoma
Bilateral Calcific Retina Arteriolar Occlusions in a Patient with Metastatic Ovarian Carcinoma
Dec 10 2020 by McGill University Health Centre
47-year-old female with cough and fever. Imaging showed a right pulmonary infiltrate. Transbronchial needle biopsy revealed lymphangitic spread of papillary adenocarcinoma with psammoma bodies (MRI of thyroid, CT of abdomen and pelvis were negative) gynecologic evaluation negative at that time . The patient had bilateral floaters, VA: 20/40 OD and 20/20 OS. Fundus examination showed retinal arteriolar sheathing and a flat choroidal lesion OS and vitritis OD. Fluorescein angiogram showed staining of left superior temporal retinal arterioles and bilateral midperipheral patchy hyperfluorescence at RPE The patient vision in the OD deteriorated to 20/400, and in the OS 20/50. Four months later a new choroidal lesion was diagnosed OS. An abdominal mass consistent with a cystadenoma of the ovary was diagnosed. After a year patient developed systemic metastasis. Autopsy: Metastatic adenocarcinoma to the lung, both adrenals, para-aortic lymph nodes, left hip, right breast, occipital skin, serosal surface of liver, pituitary. In almost all metastatic lesions psammoma bodies were found. Presumptive diagnosis is a primary tumor of the ovary. Histopathologic examination of both eyes disclosed : Bilateral metastatic adenocarcinoma to the vitreous with partially calcified proliferation along internal limiting membrane, OS. Metastatic adenocarcinoma to choroid, OS. Bilateral optic atrophy secondary to retinal arteriolar occlusion with calcification.
Condition/keywords: bilateral, calcification, histopathology, metastatic adenocarcinoma, pathology, retinal arteriolar occlusion
-
 Bilateral Calcific Retina Arteriolar Occlusions in a Patient with Metastatic Ovarian Carcinoma
Bilateral Calcific Retina Arteriolar Occlusions in a Patient with Metastatic Ovarian Carcinoma
Dec 10 2020 by McGill University Health Centre
47-year-old female with cough and fever. Imaging showed a right pulmonary infiltrate. Transbronchial needle biopsy revealed lymphangitic spread of papillary adenocarcinoma with psammoma bodies (MRI of thyroid, CT of abdomen and pelvis were negative) gynecologic evaluation negative at that time . The patient had bilateral floaters, VA: 20/40 OD and 20/20 OS. Fundus examination showed retinal arteriolar sheathing and a flat choroidal lesion OS and vitritis OD. Fluorescein angiogram showed staining of left superior temporal retinal arterioles and bilateral midperipheral patchy hyperfluorescence at RPE. The patient vision in the OD deteriorated to 20/400, and in the OS 20/50. Four months later a new choroidal lesion was diagnosed OS. An abdominal mass consistent with a cystadenoma of the ovary was diagnosed. After a year patient developed systemic metastasis. Autopsy: Metastatic adenocarcinoma to the lung, both adrenals, para-aortic lymph nodes, left hip, right breast, occipital skin, serosal surface of liver, pituitary. In almost all metastatic lesions psammoma bodies were found. Presumptive diagnosis is a primary tumor of the ovary. Histopathologic examination of both eyes disclosed : Bilateral metastatic adenocarcinoma to the vitreous with partially calcified proliferation along internal limiting membrane, OS. Metastatic adenocarcinoma to choroid, OS. Bilateral optic atrophy secondary to retinal arteriolar occlusion with calcification.
Condition/keywords: bilateral, calcification, histopathology, metastatic adenocarcinoma, pathology, retinal arteriolar occlusion
-
 Bilateral Calcific Retina Arteriolar Occlusions in a Patient with Metastatic Ovarian Carcinoma
Bilateral Calcific Retina Arteriolar Occlusions in a Patient with Metastatic Ovarian Carcinoma
Dec 10 2020 by McGill University Health Centre
47-year-old female with cough and fever. Imaging showed a right pulmonary infiltrate. Transbronchial needle biopsy revealed lymphangitic spread of papillary adenocarcinoma with psammoma bodies (MRI of thyroid, CT of abdomen and pelvis were negative) gynecologic evaluation negative at that time Patient had bilateral floaters, VA: 20/40 OD and 20/20 OS. Fundus examination showed retinal arteriolar sheathing and a flat choroidal lesion OS and vitritis OD. Fluorescein angiogram showed staining of left superior temporal retinal arterioles and bilateral midperipheral patchy hyperfluorescence at RPE The patient vision in the OD deteriorated to 20/400, and in the OS 20/50. Four months later a new choroidal lesion was diagnosed OS. An abdominal mass consistent with a cystadenoma of the ovary was diagnosed. After a year patient developed systemic metastasis. Autopsy: Metastatic adenocarcinoma to the lung, both adrenals, para-aortic lymph nodes, left hip, right breast, occipital skin, serosal surface of liver, pituitary. In almost all metastatic lesions psammoma bodies were found. Presumptive diagnosis is a primary tumor of the ovary. Histopathologic examination of both eyes disclosed : Bilateral metastatic adenocarcinoma to the vitreous with partially calcified proliferation along internal limiting membrane, OS. Metastatic adenocarcinoma to choroid, OS. Bilateral optic atrophy secondary to retinal arteriolar occlusion with calcification.
Condition/keywords: bilateral, calcification, histopathology, metastatic adenocarcinoma, pathology, retinal arteriolar occlusion
-
 Bilateral Calcific Retina Arteriolar Occlusions in a Patient with Metastatic Ovarian Carcinoma
Bilateral Calcific Retina Arteriolar Occlusions in a Patient with Metastatic Ovarian Carcinoma
Dec 10 2020 by McGill University Health Centre
47-year-old female with cough and fever. Imaging showed a right pulmonary infiltrate. Transbronchial needle biopsy revealed lymphangitic spread of papillary adenocarcinoma with psammoma bodies (MRI of thyroid, CT of abdomen and pelvis were negative) gynecologic evaluation negative at that time . The patient had bilateral floaters, VA: 20/40 OD and 20/20 OS. Fundus examination showed retinal arteriolar sheathing and a flat choroidal lesion OS and vitritis OD. Fluorescein angiogram showed staining of left superior temporal retinal arterioles and bilateral midperipheral patchy hyperfluorescence at RPE The patient vision in the OD deteriorated to 20/400, and in the OS 20/50. Four months later a new choroidal lesion was diagnosed OS. An abdominal mass consistent with a cystadenoma of the ovary was diagnosed. After a year patient developed systemic metastasis. Autopsy: Metastatic adenocarcinoma to the lung, both adrenals, para-aortic lymph nodes, left hip, right breast, occipital skin, serosal surface of liver, pituitary. In almost all metastatic lesions psammoma bodies were found. Presumptive diagnosis is a primary tumor of the ovary. Histopathologic examination of both eyes disclosed : Bilateral metastatic adenocarcinoma to the vitreous with partially calcified proliferation along internal limiting membrane, OS. Metastatic adenocarcinoma to choroid, OS. Bilateral optic atrophy secondary to retinal arteriolar occlusion with calcification.
Condition/keywords: bilateral, calcification, histopathology, metastatic adenocarcinoma, pathology, retinal arteriolar occlusion
-
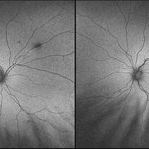
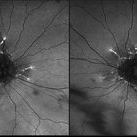
 Bilateral Calcific Retina Arteriolar Occlusions in a Patient with Metastatic Ovarian Carcinoma
Bilateral Calcific Retina Arteriolar Occlusions in a Patient with Metastatic Ovarian Carcinoma
Dec 10 2020 by McGill University Health Centre
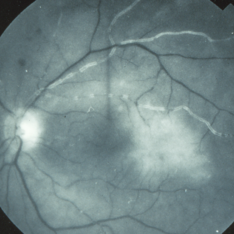
47-year-old female with cough and fever. Imaging showed a right pulmonary infiltrate. Transbronchial needle biopsy revealed lymphangitic spread of papillary adenocarcinoma with psammoma bodies (MRI of thyroid, CT of abdomen and pelvis were negative) gynecologic evaluation negative at that time . The patient had bilateral floaters, VA: 20/40 OD and 20/20 OS. Fundus examination showed retinal arteriolar sheathing and a flat choroidal lesion OS and vitritis OD. Fluorescein angiogram showed staining of left superior temporal retinal arterioles and bilateral midperipheral patchy hyperfluorescence at RPE. The patient vision in the OD deteriorated to 20/400, and in the OS 20/50. Four months later a new choroidal lesion was diagnosed OS. An abdominal mass consistent with a cystadenoma of the ovary was diagnosed. After a year patient developed systemic metastasis. Autopsy: Metastatic adenocarcinoma to the lung, both adrenals, para-aortic lymph nodes, left hip, right breast, occipital skin, serosal surface of liver, pituitary. In almost all metastatic lesions psammoma bodies were found. Presumptive diagnosis is a primary tumor of the ovary.
Imaging device: Fluoroscein angiogram
Condition/keywords: bilateral, calcification, metastatic adenocarcinoma, retinal arteriolar occlusion
-
 Bilateral Calcific Retina Arteriolar Occlusions in a Patient with Metastatic Ovarian Carcinoma
Bilateral Calcific Retina Arteriolar Occlusions in a Patient with Metastatic Ovarian Carcinoma
Dec 10 2020 by McGill University Health Centre
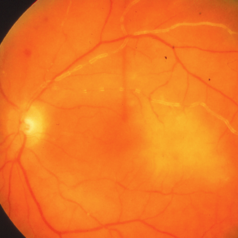
47-year-old female with cough and fever. Imaging showed a right pulmonary infiltrate. Transbronchial needle biopsy revealed lymphangitic spread of papillary adenocarcinoma with psammoma bodies. MRI of thyroid, CT of abdomen and pelvis were negative. gynecologic evaluation negative at that time . The patient had bilateral floaters, VA: 20/40 OD and 20/20 OS. Fundus examination showed retinal arteriolar sheathing and a flat choroidal lesion OS and vitritis OD. Fluorescein angiogram showed staining of left superior temporal retinal arterioles and bilateral midperipheral patchy hyperfluorescence at RPE The patient vision in the OD deteriorated to 20/400, and in the OS 20/50. Four months later a new choroidal lesion was diagnosed OS. An abdominal mass consistent with a cystadenoma of the ovary was diagnosed. After a year patient developed systemic metastasis. Autopsy: Metastatic adenocarcinoma to the lung, both adrenals, para-aortic lymph nodes, left hip, right breast, occipital skin, serosal surface of liver, pituitary. In almost all metastatic lesions psammoma bodies were found. Presumptive diagnosis is a primary tumor of the ovary.
Condition/keywords: bilateral, calcification, metastatic adenocarcinoma, retinal arteriolar occlusion
-
 Bilateral Lymphoma Metastasis after Resolution with IVM
Bilateral Lymphoma Metastasis after Resolution with IVM
Sep 19 2018 by Olivia Rainey
Ultra-wide field, pseudocolor fundus images of an 86-year-old female treated with intravitreal methothrexate as a management of subretinal infiltrate in the macula of the right eye, as a manifestation of leukemia. Her last intravitreal methotrexate injection was 5/1/18.
Photographer: Olivia Rainey
Imaging device: Optos
Condition/keywords: bilateral, leukemia, methotrexate, Optos, pseudocolor, ultra-wide field imaging, uveitis
-
 Bilateral Lymphoma Metastasis after Resolution with IVM
Bilateral Lymphoma Metastasis after Resolution with IVM
Sep 19 2018 by Olivia Rainey
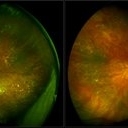
Ultra-wide field, autofluorescence images of an 86-year-old female treated with intravitreal methothrexate as a management of subretinal infiltrate in the macula of the right eye, as a manifestation of leukemia. Her last intravitreal methotrexate injection was 5/1/18.
Photographer: Olivia Rainey
Imaging device: Optos
Condition/keywords: bilateral, fundus autofluorescence (FAF), lymphoma, Optos, ultra-wide field imaging, uveitis
-
 Congenital Hypertrophy of the Retinal Pigment Epithelium
Congenital Hypertrophy of the Retinal Pigment Epithelium
Nov 11 2019 by Jessica Norkus
Bilateral Optos ultra wide field imaging of a 31-year-old female patient with CHRPE lesions. Lesions in OD were suspicious of Gardner Syndrome due to familial history of cancerous polyps in colon. Patient underwent colonoscopy and was deemed clear.
Photographer: Jessica Norkus, COA, Retina Specialists of Michigan
Imaging device: Optos Ultra Wide Field Camera
Condition/keywords: bear tracks, bilateral, color fundus photograph, color photo, congenital hypertrophy of the retinal pigment epithelium (CHRPE), fundus autofluorescence (FAF), fundus photograph, lacunae, macula, optic disc, Optos, pseudocolor, ultra-wide field imaging
-
 Congenital Retinal Pigment Epithelial Hypertrophy (CHRPE) Associated with Gardner's Syndrome
Congenital Retinal Pigment Epithelial Hypertrophy (CHRPE) Associated with Gardner's Syndrome
Mar 13 2018 by Olivia Rainey
Ultra-wide field fundus autofluorescence images of a 14-year-old patient with congenital retinal pigment epithelial hypertrophy affecting both eyes as a manifestation of Gardner's Syndrome.
Photographer: Olivia Rainey
Imaging device: Optos
Condition/keywords: bilateral, familial adenomatous polyposis, fundus autofluorescence (FAF), Gardner Syndrome, hypofluorescent lesions, Optos, ultra-wide field imaging
-
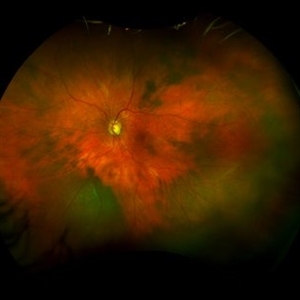 Diffuse uveal melanoma
Diffuse uveal melanoma
Dec 25 2022 by Giovanni Cuffaro, MD
Left eye of a bilateral diffuse uveal melanoma with liver metastases. Complete monosomy 3 and HLA-A*0201–positive was detected.
Photographer: Giovanni Cuffaro, Università Cattolica del Sacro Cuore, Fondazione Policlinico A. Gemelli IRCCS
Imaging device: California from Optos
Condition/keywords: Bilateral, Diffuse Choroidal Melanoma, Monosomy 3
-
 Elmiron Toxicity
Elmiron Toxicity
Jan 12 2018 by Jessica Norkus
Bilateral ultra-wide field pseudo-color and autofluorescent images of a 46-year-old female with Elmiron Toxicity.
Photographer: Jessica Norkus
Imaging device: Optos
Condition/keywords: autofluorescence imaging, bilateral, color fundus photograph, drug toxicity, Optos, toxic maculopathy, toxic retinopathy, ultra-wide field imaging
-
Figure: Bilateral Sclerosis of Retinal Vessels
Apr 22 2020 by Padmaja Kumari Rani, M.S, FICO,FRCS
Fundus photographs of an 71 -year-old women with bilateral sclerosed vessels s/p bilateral CRVO with PRP laser marks in the left eye. Known diabetic and hypertensive. Her visual acuity is good inspite of extensive sclerosis of vessles in both eyes - 20/30, N6 in the right eye and 20/80, N6 in the left eye.
Photographer: Batchanaboina subba rao
Imaging device: Optos widefield fundus camera
Condition/keywords: bilateral, retinal vessel
-
 Macular Degeneration with Significant Drusen
Macular Degeneration with Significant Drusen
Jul 10 2018 by Karen Panzegrau
Zoomed-in ultra-wide field images of a 77-year-old female with macular degeneration with significant drusen.
Photographer: Karen Panzegrau
Imaging device: Optos
Condition/keywords: age-related macular degeneration (AMD), bilateral, drusen, fundus photograph, pseudocolor
-
 Macular Pattern Dystrophy Associated with MELAS
Macular Pattern Dystrophy Associated with MELAS
Dec 19 2019 by Olivia Rainey
Bilateral wide field pseudocolor images of a 54-year-old female with macular pattern dystrophy associated with MELAS. The patient is positive for m.3243A>G in MT-TL1. She had stroke in her 40s, hearing loss in her 30s, and has early onset diabetes. MyRetinaTracker shows VUS in RP1L1. Mutation in RP1L1 have been describe in other families with occult macular dystrophy. Farnsworth D15 is showing mild tritan abnormality, which is most commonly seen with acquired maculopathies. 12/17/19 patient's Optos and OCT show mild progression of atrophy.
Photographer: Olivia Rainey
Imaging device: Optos California
Condition/keywords: advanced geographic atrophy, bilateral, fundus photograph, MELAS, Optos, pattern macular dystrophy, pseudocolor, wide angle imaging
-
 Macular Pattern Dystrophy Associated with MELAS
Macular Pattern Dystrophy Associated with MELAS
Dec 19 2019 by Olivia Rainey
Bilateral wide field fundus autofluorescence images of a 54-year-old female with macular pattern dystrophy associated with MELAS. The patient is positive for m.3243A>G in MT-TL1. She had stroke in her 40s, hearing loss in her 30s, and has early onset diabetes. MyRetinaTracker shows VUS in RP1L1. Mutation in RP1L1 have been describe in other families with occult macular dystrophy. Farnsworth D15 is showing mild tritan abnormality, which is most commonly seen with acquired maculopathies. 12/17/19 patient's Optos and OCT show mild progression of atrophy.
Photographer: Olivia Rainey
Imaging device: Optos California
Condition/keywords: advanced geographic atrophy, bilateral, fundus autofluorescence (FAF), MELAS, Optos, pattern macular dystrophy, wide angle imaging
-
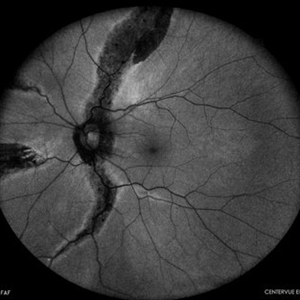 Pigmented Paravenous Retinochoroidal Atrophy
Pigmented Paravenous Retinochoroidal Atrophy
Oct 1 2023 by Bruno DECAY, MD
Fundus photograph (autofluorescence) of a 43-year-old myopic man (left eye) Axial length: 29.32 mm
Photographer: Bruno DECAY, MD
Imaging device: iCARE EIDON confocal fundus imaging system (Ultra-Widefield Module)
Condition/keywords: Bilateral, High myopia
-
 Pigmented Paravenous Retinochoroidal Atrophy
Pigmented Paravenous Retinochoroidal Atrophy
Oct 1 2023 by Bruno DECAY, MD
Fundus photograph of a 43-year-old myopic man (left eye) Axial length: 29.32 mm
Photographer: Bruno DECAY, MD
Imaging device: iCARE EIDON confocal fundus imaging system (Ultra-Widefield Module)
Condition/keywords: Bilateral, High myopia, Pigmented Paravenous Retinochoroidal Atrophy
-
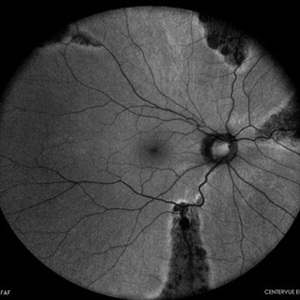 Pigmented Paravenous Retinochoroidal Atrophy
Pigmented Paravenous Retinochoroidal Atrophy
Oct 1 2023 by Bruno DECAY, MD
Fundus photograph (autofluorescence) of a 43-year-old myopic man (right eye) Axial length: 27.67 mm
Photographer: Bruno DECAY, MD
Imaging device: iCARE EIDON confocal fundus imaging system (Ultra-Widefield Module)
Condition/keywords: Bilateral, High Myopia, Pigmented Paravenous Retinochoroidal Atrophy
-
 Pigmented Paravenous Retinochoroidal Atrophy
Pigmented Paravenous Retinochoroidal Atrophy
Oct 1 2023 by Bruno DECAY, MD
Fundus photograph of a 43-year-old myopic man (right eye) Axial length: 27.67 mm
Photographer: Bruno DECAY, MD
Imaging device: iCARE EIDON confocal fundus imaging system (Ultra-Widefield Module)
Condition/keywords: Bilateral, High myopia, Pigmented Paravenous Retinochoroidal Atrophy
-
 Purtscher's Retinopathy
Purtscher's Retinopathy
Mar 30 2018 by Olivia Rainey
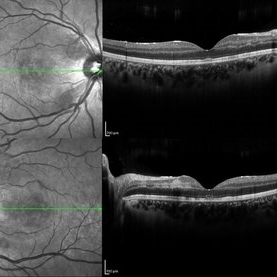
Bilateral OCTS of a 21-year-old female with Purtscher's Retinopathy affecting both eyes. Patient developed acute pancreatitis triggered by hypercalcemia and likely increased alcohol consumption.
Photographer: Olivia Rainey
Imaging device: Spectralis
Condition/keywords: acute pancreatitis, bilateral, optical coherence tomography (OCT), Purtscher's retinopathy
-
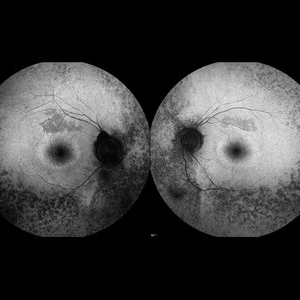 Retinitis Pigmentosa
Retinitis Pigmentosa
May 27 2016 by Olivia Rainey
Bilateral fundus autofluorescence images of retinitis pigmentosa.
Photographer: Olivia Rainey
Imaging device: Heidelberg Spectralis
Condition/keywords: 50 degrees, bilateral, fundus autofluorescence (FAF), hereditary retinal dystrophy, retinitis pigmentosa
-
 Sturge-Weber Syndrome
Sturge-Weber Syndrome
Nov 17 2023 by Zach Seim
Topcon photo of a 37 year old female with Sturge-Weber syndrome affecting OU. Patient presents with prominent episcleral vasculature and DCC 20/20 VA OU. Plan to monitor.
Photographer: Zach Seim
Imaging device: Topcon 50DX
Condition/keywords: bilateral, external, external photography, left eye, right eye, Sturge-Weber syndrome, Topcon
-
Antiphospholipid Antibody Syndrome
Feb 10 2016 by Mallika Goyal, MD
Bilateral extensive retinal vascular occlusion in a 25-year-old lady with antiphospholipid antibody syndrome following resolution of hypertensive retinopathy grade 4 . She had recurrent abortions and recently resolved papilledema from idiopathic raised intracranial pressure.
Photographer: Mallika Goyal, MD, Apollo Health City, Hyderabad, India
Condition/keywords: antiphospholipid antibody syndrome

 Loading…
Loading…