Search results (181 results)
-
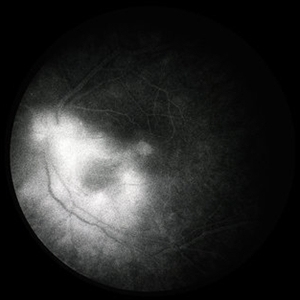
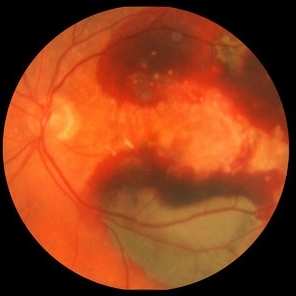 ARMD with Subretinal Hemorrhages and Macular Scarring
ARMD with Subretinal Hemorrhages and Macular Scarring
Oct 16 2012 by Jeffrey G. Gross, MD, FASRS
ARMD with subretinal hemorrhages and macular scarring, 20/400.
Condition/keywords: 20/400, macular scar, subretinal hemorrhage
-
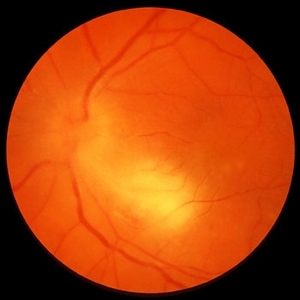
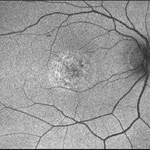
 Macular Hole
Macular Hole
Sep 27 2012 by Jeffrey G. Gross, MD, FASRS
Macular hole, 20/400.
Condition/keywords: 20/400, macular hole
-
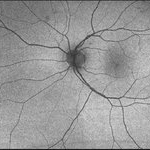
 Macular Pucker
Macular Pucker
Oct 8 2012 by Jeffrey G. Gross, MD, FASRS
Macular pucker, 20/400.
Condition/keywords: 20/400, macular pucker
-
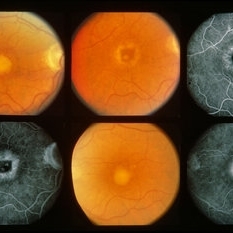
 Sarcoid Granuloma of Optic Nerve
Sarcoid Granuloma of Optic Nerve
Oct 9 2012 by Jeffrey G. Gross, MD, FASRS
Sarcoid granuloma of optic nerve, 20/400.
Condition/keywords: 20/400, autoimmunity, sarcoid granuloma, sarcoidosis
-
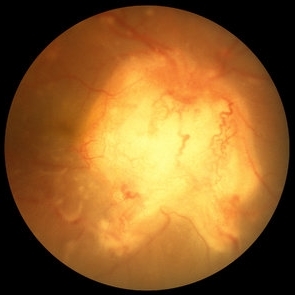
 Sarcoid Granuloma of Optic Nerve
Sarcoid Granuloma of Optic Nerve
Oct 9 2012 by Jeffrey G. Gross, MD, FASRS
Sarcoid granuloma of optic nerve, FA, early phase, 20/400.
Condition/keywords: 20/400, autoimmunity, early phase, sarcoid granuloma, sarcoidosis
-
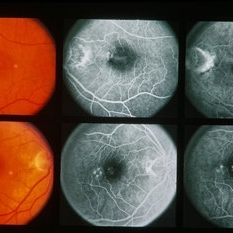
 Toxoplasmosis Chorioretinitis
Toxoplasmosis Chorioretinitis
Oct 10 2012 by Jeffrey G. Gross, MD, FASRS
Toxoplasmosis chorioretinitis, 20/400, + APD.
Condition/keywords: 20/400, afferent pupillary defect (APD), toxoplasmosis chorioretinitis
-
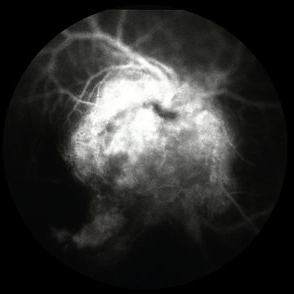
 Toxoplasmosis Chorioretinitis
Toxoplasmosis Chorioretinitis
Oct 10 2012 by Jeffrey G. Gross, MD, FASRS
Toxoplasmosis chorioretinitis, 20/400, + APD, FA late phase.
Condition/keywords: 20/400, afferent pupillary defect (APD), FA late phase, toxoplasmosis chorioretinitis
-
---thumb.jpg/image-square;max$300,300.ImageHandler) "Spots" In The Central Visual Zone
"Spots" In The Central Visual Zone
Oct 14 2013 by Maurice F. Rabb
A 26 year old healthy female who had been aware of decreased vision in OS for 5 days before the initial examination. When questioned specifically about OD, she did admit to being aware of some "spots" in the central visual zone. Her past ocular history is negative for eye disease and the family history is negative for retinal and macular disease. The patient is in excellent general health. She had a recent upper respiratory infection and is presently disabled because of a herniated disc. Uncorrected vision OD is 20/20 and OS is 20/400, improving to 20/100- with pinhole. The findings of significance are noted in the posterior poles.
Condition/keywords: spots in the central visual zone
-
---thumb.jpg/image-square;max$300,300.ImageHandler) "Spots" In The Central Visual Zone
"Spots" In The Central Visual Zone
Oct 14 2013 by Maurice F. Rabb
A 26 year old healthy female who had been aware of decreased vision in OS for 5 days before the initial examination. When questioned specifically about OD, she did admit to being aware of some "spots" in the central visual zone. Her past ocular history is negative for eye disease and the family history is negative for retinal and macular disease. The patient is in excellent general health. She had a recent upper respiratory infection and is presently disabled because of a herniated disc. Uncorrected vision OD is 20/20 and OS is 20/400, improving to 20/100- with pinhole. The findings of significance are noted in the posterior poles.
Condition/keywords: spots in the central visual zone
-
---thumb.jpg/image-square;max$300,300.ImageHandler) "Spots" In The Central Visual Zone
"Spots" In The Central Visual Zone
Oct 14 2013 by Maurice F. Rabb
A 26 year old healthy female who had been aware of decreased vision in OS for 5 days before the initial examination. When questioned specifically about OD, she did admit to being aware of some "spots" in the central visual zone. Her past ocular history is negative for eye disease and the family history is negative for retinal and macular disease. The patient is in excellent general health. She had a recent upper respiratory infection and is presently disabled because of a herniated disc. Uncorrected vision OD is 20/20 and OS is 20/400, improving to 20/100- with pinhole. The findings of significance are noted in the posterior poles.
Condition/keywords: spots in the central visual zone
-
---thumb.jpg/image-square;max$300,300.ImageHandler) "Spots" In The Central Visual Zone
"Spots" In The Central Visual Zone
Oct 14 2013 by Maurice F. Rabb
A 26 year old healthy female who had been aware of decreased vision in OS for 5 days before the initial examination. When questioned specifically about OD, she did admit to being aware of some "spots" in the central visual zone. Her past ocular history is negative for eye disease and the family history is negative for retinal and macular disease. The patient is in excellent general health. She had a recent upper respiratory infection and is presently disabled because of a herniated disc. Uncorrected vision OD is 20/20 and OS is 20/400, improving to 20/100- with pinhole. The findings of significance are noted in the posterior poles.
Condition/keywords: spots in the central visual zone
-
 01 Unilateral Acute Idiopathic Maculopathy (UAIM) Pseudocolor Photograph OD
01 Unilateral Acute Idiopathic Maculopathy (UAIM) Pseudocolor Photograph OD
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of pt's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, patient mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT , diagnosed with CSCR and referred for retina evaluation. - ROS/ PMHx: negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - pseudocolor and FAF photos: RPE changes/ clumps with GA and stippled autofluorescense OD, unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, subfoveal ellipsoid zone atrophy with intact ELM with no CME or SRF OD, unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG and VF - patient rescheduled
Imaging device: Optos - California
Condition/keywords: unilateral acute idiopathic maculopathy
-
 02 Unilateral Acute Idiopathic Maculopathy (UAIM) - Pseudocolor Photograph OS
02 Unilateral Acute Idiopathic Maculopathy (UAIM) - Pseudocolor Photograph OS
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of pt's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, pt mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT , diagnosed with CSCR and referred for retina evaluation. - ROS/ PMHx: Negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - Pseudocolor and FAF photos: RPE changes/ clumps w/ GA and stippled autofluorescense OD, unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, Subfoveal ellipsoid zone atrophy w/ intact ELM W/No CME or SRF OD, Unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG & VF - patient rescheduled
Imaging device: Optos - California
Condition/keywords: unilateral acute idiopathic maculopathy
-
02123-20190508-171643-Fluorescein-R-001
Aug 26 2019 by Narciso F. Atienza, MD, MBA, FASRS, FPCS, FPAO.
47-year-old female who came in with blurring of vision of the right eye of 2 weeks duration. She is hypertensive with poor control, taking Amlodipine irregularly. Denies any cardiac problem non-diabetic. Vision upon presentation was 20/400 (OD), 20/20 (OS) . Early arterial phase shows beginning asymmetrical perfusion of the supero-temporal arcade supplying the macula. Infero-temporal arcade shows no perfusion.
Photographer: Narciso F Atienza, Jr. MD, MBA
Imaging device: Topcon TRC
Condition/keywords: asymmetrical perfusion, inferotemporal arcade, superotemporal arcade
-
 03- Unilateral Acute Idiopathic Maculopathy (UAIM) - FAF OD
03- Unilateral Acute Idiopathic Maculopathy (UAIM) - FAF OD
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of patient's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, pt mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT , diagnosed w/ CSCR and referred for retina evaluation. - ROS/ PMHx: Negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - Pseudocolor & FAF photos: RPE changes/ clumps with GA and stippled autofluorescense OD, Unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, subfoveal ellipsoid zone atrophy with intact ELM with no CME or SRF OD, unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG & VF - pt rescheduled!
Imaging device: Optos - California
Condition/keywords: unilateral acute idiopathic maculopathy
-
 04- Unilateral Acute Idiopathic Maculopathy (UAIM) - FAF OS
04- Unilateral Acute Idiopathic Maculopathy (UAIM) - FAF OS
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of pateint's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, patient mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT, diagnosed with CSCR and referred for retina evaluation. - ROS/ PMHx: negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - pseudocolor and FAF photos: RPE changes/ clumps with GA & stippled autofluorescence OD, unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, subfoveal ellipsoid zone atrophy with intact ELM with no CME or SRF OD, unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG & VF - patient rescheduled
Imaging device: Optos - California
Condition/keywords: unilateral acute idiopathic maculopathy
-
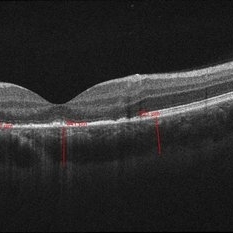 05- Unilateral Acute Idiopathic Maculopathy (UAIM) - OCT OD
05- Unilateral Acute Idiopathic Maculopathy (UAIM) - OCT OD
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of pt's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, pt mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT , diagnosed with CSCR and referred for retina evaluation. - ROS/ PMHx: Negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - Pseudocolor and FAF photos: RPE changes/ clumps w/ GA and stippled autofluorescense OD, unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, Subfoveal ellipsoid zone atrophy w/ intact ELM W/No CME or SRF OD, Unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG & VF - patient rescheduled
Imaging device: Zeiss-Cirrus 4000
Condition/keywords: unilateral acute idiopathic maculopathy
-
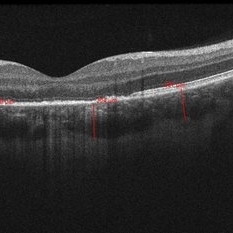 05- Unilateral Acute Idiopathic Maculopathy (UAIM) - OCT OD2
05- Unilateral Acute Idiopathic Maculopathy (UAIM) - OCT OD2
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of pt's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, pt mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT , diagnosed with CSCR and referred for retina evaluation. - ROS/ PMHx: Negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - Pseudocolor and FAF photos: RPE changes/ clumps w/ GA and stippled autofluorescense OD, unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, Subfoveal ellipsoid zone atrophy w/ intact ELM W/No CME or SRF OD, Unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG & VF - patient rescheduled
Imaging device: Zeiss-Cirrus 4000
Condition/keywords: unilateral acute idiopathic maculopathy
-
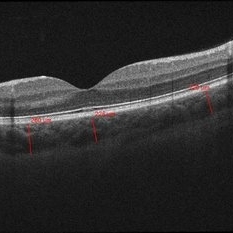 06- Unilateral Acute Idiopathic Maculopathy (UAIM) - OCT OS
06- Unilateral Acute Idiopathic Maculopathy (UAIM) - OCT OS
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of pt's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, pt mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT , diagnosed with CSCR and referred for retina evaluation. - ROS/ PMHx: Negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - Pseudocolor and FAF photos: RPE changes/ clumps w/ GA and stippled autofluorescense OD, unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, Subfoveal ellipsoid zone atrophy w/ intact ELM W/No CME or SRF OD, Unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG & VF - patient rescheduled
Imaging device: Zeiss-Cirrus 4000
Condition/keywords: unilateral acute idiopathic maculopathy
-
Accordioning Crystalline Lens
Jul 8 2013 by Jason S. Calhoun
71-year-old male complained of blurred vision in the left eye. VA 20/40, right eye and 20/400, left eye without correction. Slit lamp exam shows Crystalline lens in both eyes. Right eye IOL is aligned and centered. Left eye shows an accordion of the crystalline lens. Retro illumination shows the IOL bent inward in the left eye. There was a 6-diopter difference of astigmatism between the right and left eye. Patient will have surgery to correct the issue.
Photographer: Jason S. Calhoun, Department of Ophthalmology, Mayo Clinic Jacksonville, Florida
Condition/keywords: dislocated crystalline lens
-
Accordioning Crystalline Lens
Jul 8 2013 by Jason S. Calhoun
71-year-old male complained of blurred vision in the left eye. VA 20/40, right eye and 20/400, left eye without correction. Slit lamp exam shows Crystalline lens, both eyes. Right eye IOL is aligned and centered. Left eye shows an accordion of the crystalline lens. Retro illumination shows the IOL bent inward in the left eye. There was a 6-diopter difference of astigmatism between the right and left eye. Patient will have surgery to correct the issue.
Photographer: Jason S. Calhoun, Department of Ophthalmology, Mayo Clinic Jacksonville, Florida
Condition/keywords: dislocated crystalline lens
-
Accordioning Crystalline Lens
Jul 8 2013 by Jason S. Calhoun
71-year-old male complained of blurred vision in the left eye. VA 20/40, right eye and 20/400, left eye without correction. Slit lamp exam shows Crystalline lens in both eyes. Right eye IOL is aligned and centered. Left eye shows an accordion of the crystalline lens. Retro Illumination shows the IOL bent inward in the left eye. There was a 6-diopter difference of astigmatism between the right and left eye. Patient will have surgery to correct the issue.
Photographer: Jason S. Calhoun, Department of Ophthalmology, Mayo Clinic Jacksonville, Florida
Condition/keywords: dislocated crystalline lens
-
 AMPPPE
AMPPPE
Apr 17 2013 by Howard Schatz, MD
III AMPPPE-TB; right eye: 20/60; left eye: 20/400.
Condition/keywords: acute posterior multifocal placoid pigment epitheliopathy (APMPPE), tuberculosis
-
 AOFPED
AOFPED
Dec 9 2014 by Howard Schatz, MD
70-year-old female. AOFPED. RE 20/60 LE 20/400.
Condition/keywords: AOFPED
-
 AOFPED
AOFPED
Dec 9 2014 by Howard Schatz, MD
72-year-old white female. AOFPED. RE 20/400 LE 20/250.
Condition/keywords: AOFPED

 Loading…
Loading…