Search results (249 results)
-
 Acute Posterior Multifocal Placoid Pigment Epitheliopathy
Acute Posterior Multifocal Placoid Pigment Epitheliopathy
Feb 20 2024 by Soobien Lee
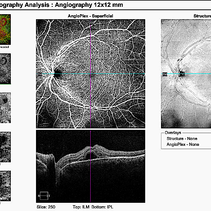
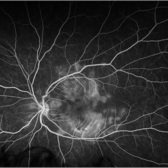
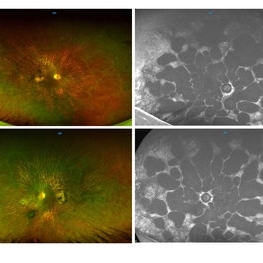
12x12mm OCT Angiography of a 20-year-old caucasian female with viral prodrome and vision loss OS>OD secondary to Acute Posterior Multifocal Placoid Pigment Epitheliopathy (APPME). Imaging shows multifocal flow voids.
Photographer: Kim Seay, Elman Retina Group
Imaging device: 12x12mm OCT-Angiography
Condition/keywords: acute posterior multifocal placoid pigment epitheliopathy (APMPPE), bacillary layer detachment, OCT, OCT Angiography, Uveitis, white dot syndrome
-
 Acute Posterior Multifocal Placoid Pigment Epitheliopathy
Acute Posterior Multifocal Placoid Pigment Epitheliopathy
Feb 20 2024 by Soobien Lee
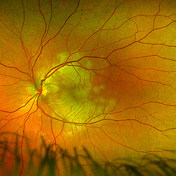
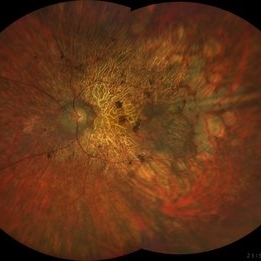
Optos color fundus photograph of a 20-year-old caucasian female with viral prodrome and vision loss OS>OD secondary to Acute Posterior Multifocal Placoid Pigment Epitheliopathy (APPME). Imaging of her left eye shows multiple bilateral creamy yellow-white placoid lesions at the level of RPE and choroid throughout the posterior pole.
Photographer: Ashley Metzger, Elman Retina Group
Imaging device: Optos Ultra-Widefield Imaging
Condition/keywords: acute posterior multifocal placoid pigment epitheliopathy (APMPPE), bacilliary layer detachment, Optos, uveitis, white dot syndrome
-
 Acute Posterior Multifocal Placoid Pigment Epitheliopathy
Acute Posterior Multifocal Placoid Pigment Epitheliopathy
Feb 20 2024 by Soobien Lee
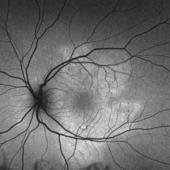
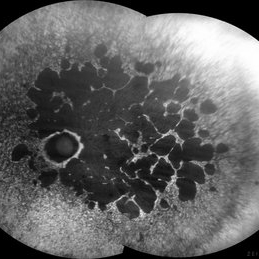
Optos fundus autofluorescence photograph of a 20-year-old caucasian female with viral prodrome and vision loss OS>OD secondary to Acute Posterior Multifocal Placoid Pigment Epitheliopathy (APPME). Imaging of her left eye shows hypoautofluorescent areas corresponding to multiple bilateral placoid lesions at the level of RPE and choroid throughout the posterior pole.
Photographer: Ashley Metzger, Elman Retina Group
Imaging device: Optos Ultra-Widefield Autoflurescence Imaging
Condition/keywords: acute posterior multifocal placoid pigment epitheliopathy (APMPPE), autofluorescence imaging, bacilliary layer detachment, Optos, OPTOS CALIFORNIA, uveitis, white dot syndrome
-
 Acute Posterior Multifocal Placoid Pigment Epitheliopathy
Acute Posterior Multifocal Placoid Pigment Epitheliopathy
Feb 20 2024 by Soobien Lee
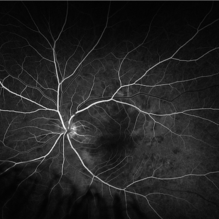
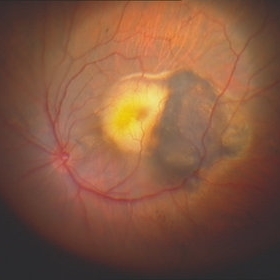
Fluorescein angiogram of a 20-year-old caucasian female with viral prodrome and vision loss OS>OD secondary to Acute Posterior Multifocal Placoid Pigment Epitheliopathy (APPME). Early blockage with late hyperfluorescent leakage can be seen on fluorescein angiography of the left eye.
Photographer: Ashley Metzger, Elman Retina Group
Imaging device: Optos Ultra-Widefield Fluorescein Angiography
Condition/keywords: acute posterior multifocal placoid pigment epitheliopathy (APMPPE), bacilliary layer detachment, FA, FA early phase, fluorescein angiogram (FA), Optos, uveitis, white dot syndrome
-
 Acute Posterior Multifocal Placoid Pigment Epitheliopathy
Acute Posterior Multifocal Placoid Pigment Epitheliopathy
Feb 20 2024 by Soobien Lee
Fluorescein angiogram of a 20-year-old caucasian female with viral prodrome and vision loss OS>OD secondary to Acute Posterior Multifocal Placoid Pigment Epitheliopathy (APPME). Early blockage with late hyperfluorescent leakage can be seen on fluorescein angiography of the left eye.
Photographer: Ashley Metzger, Elman Retina Group
Imaging device: Optos Ultra-Widefield Fluorescein Angiography
Condition/keywords: acute posterior multifocal placoid pigment epitheliopathy (APMPPE), bacilliary layer detachment, FA, FA late phase, FA late phase leakage, fluorescein angiogram (FA), Optos, uveitis, white dot syndrome
-
 Acute Posterior Multifocal Placoid Pigment Epitheliopathy
Acute Posterior Multifocal Placoid Pigment Epitheliopathy
Feb 20 2024 by Soobien Lee
A 20-year-old caucasian female with viral prodrome and vision loss OS>OD secondary to Acute Posterior Multifocal Placoid Pigment Epitheliopathy (APPME). OCT of the left macula shows bacillary layer detachment.
Photographer: Kim Seay, Elman Retina Group
Condition/keywords: acute posterior multifocal placoid pigment epitheliopathy (APMPPE), bacilliary layer detachment, OCT, Uveitis, white dot syndrome
-
 Rod Cone dystrophy
Rod Cone dystrophy
Nov 29 2022 by Niloofar Piri, MD
Fundus photograph of the left eye in a 58 yo male with rod cone dystrophy. He presented with night blindness and peripheral vision loss since youth and recent decrease in central vision for the past 10 years. Notice waxy pallor of the nerve, severe arterial narrowing and chorioretinal atrophy mainly around the arcades as well as posterior pole along with RPE hyperplastic changes and atrophy. RPE atrophy in midperiphery has coin shaped appearance. FAF has characteristic appearance (uploaded separately) He has one pathogenic variants of both CEP290 and PRPH2 genes.
Photographer: Sean Kelso, Saint Louis University
Condition/keywords: hereditary retinal deg, hereditary retinal dystrophy, Rod cone dystrophy
-
 Rod Cone dystrophy
Rod Cone dystrophy
Nov 29 2022 by Niloofar Piri, MD
Fundus autofluorescence of the left eye in a 58 yo male with rod cone dystrophy. He presented with night blindness and peripheral vision loss since youth and recent decrease in central vision for the past 10 years. Notice multiple coin shaped hypoautofluorescent pacthes within central 20 degrees which are coalescing centrally. (fundus photo uploaded separately) He has one pathogenic variants of both CEP290 and PRPH2 genes.
Photographer: Sean Kelso, Saint Louis University
Condition/keywords: hereditary retinal degeneration, hereditary retinal dystrophy, rod cone dystrophy
-
 Valsalva Retinopathy
Valsalva Retinopathy
Nov 18 2022 by Niloofar Piri, MD
Sudden vision loss immediately after severe vomiting. Color fundus photo demonstrates large sub ILM hemorrhage consistent with valsalva retinopathy.
Photographer: Sean Kelso, Saint Louis University
Condition/keywords: SUB ILM hemorrhage, sub internal limiting membrane haemorrhage, valsalva retinopathy
-
 Aggressive Posterior Retinopathy of Prematurity (APROP)
Aggressive Posterior Retinopathy of Prematurity (APROP)
May 16 2025 by KANWALJEET HARJOT MADAN, M.S. (Ophthalmology); FAICO (Vitreous - Retina)
This is the fundus picture of right eye of a premature neonate depicting Aggressive Posterior Retinopathy of Prematurity (APROP). It is a severe rapidly progressing form of retinopathy that can lead to vision loss and blindness. It requires prompt diagnosis and treatment in the form of anti-VEGF agents and laser photocoagulation.
Photographer: Dr. Kanwaljeet Harjot Madan, Thind Eye Hospital, Jalandhar City (Punjab) INDIA.
Imaging device: Zeiss Clarus
Condition/keywords: Oxygen Exposure, retinopathy of prematurity (ROP)
-
 Central Retinal Vein Occlusion
Central Retinal Vein Occlusion
Jan 21 2022 by Olivia Rainey
Ultra-widefield fluorescein angiogram of a 23-year-old female with a Central Retinal Vein Occlusion affecting her left eye. The patient presented on 12/22/2021 cc20/40-2 vision in the left eye. The patient reported recent trauma of being hit with a fist on both sides of face followed by vision loss. The patient has history of Hashimoto's thyroid disease. The following labs have been ordered, PT, PTT, CBC, antithrombin III activity, protein C, protein S, Factor V Leiden mutation, Prothrombin (G20210A), lipid panel, HbA1c, quantiferon gold, RPR, and CXR.
Photographer: Olivia Rainey, OCT-C, COA
Imaging device: Optos California
Condition/keywords: central retinal vein occlusion (CRVO), disc leakage, fluorescein angiogram (FA), fluorescein leakage, left eye, non-ischemic central retinal vein occlusion (CRVO), Optos, trauma, ultra-wide field imaging
-
 MEWDS
MEWDS
Oct 9 2020 by David L Kilpatrick, MD
26-year-old female presented with unilateral vision loss. She c/o flashes and a peripheral scotoma. Vision was 20/100. On exam, she showed foveal granularity, mild disc edema, and white dots as seen. Three weeks later, white dots had resolved and vision improved to 20/25.
Photographer: Mississippi Retina Associates
Imaging device: Optos
Condition/keywords: multiple evanescent white dot syndrome (MEWDS)
-
 Choroideremia
Choroideremia
Sep 21 2022 by Zach Seim
Ultra-widefield fundus photo of a 74 year old male presenting with severe vision loss beginning at age 55. Patient sought a second opinion with our office and was diagnosed with Choroideremia. Patient denies hearing loss, heart problems, balance issues, polydactyly, kidney problems, and dental problems. Patient reports that nobody in the family had blindness. Choroideremia is an X-linked chorioretinal dystrophy characterized by the diffuse, progressive degeneration of the retinal pigment epithelium (RPE), photoreceptors and choriocapillaris. It is caused by a mutation in the CHM gene.
Photographer: Zach Seim
Imaging device: Optos California
Condition/keywords: choroideremia, hereditary choroidal atrophy, hereditary retinal dystrophy, Optos, pseudocolor, ultra-wide field imaging
-
 Choroideremia
Choroideremia
Sep 21 2022 by Zach Seim
Ultra-widefield fundus photo of a 74 year old male presenting with severe vision loss beginning at age 55. Patient sought a second opinion with our office and was diagnosed with Choroideremia. Patient denies hearing loss, heart problems, balance issues, polydactyly, kidney problems, and dental problems. Patient reports that nobody in the family had blindness. Choroideremia is an X-linked chorioretinal dystrophy characterized by the diffuse, progressive degeneration of the retinal pigment epithelium (RPE), photoreceptors and choriocapillaris. It is caused by a mutation in the CHM gene.
Photographer: Zach Seim
Imaging device: Optos California
Condition/keywords: choroideremia, hereditary choroidal atrophy, hereditary retinal dystrophy, left eye, light perception, low vision, Optos, pseudocolor, ultra-wide field imaging
-
 Chronical Submacular Hemorrhage in the Setting of Neovascular AMD
Chronical Submacular Hemorrhage in the Setting of Neovascular AMD
Mar 23 2015 by Rita Couceiro, MD, MS
An 80-year-old male, with a history of hypertension and high cholesterol, complained of acute and painless vision loss in his left eye (OS) in the previous 5 months. On observation best corrected visual acuity in OS was hand motion. A dense vitreous opacity in OS precluded fundus examination. Ocular ultrasound revealed vitreous hemorrhage and thickening of the macular area. The patient was submitted to pars plana vitrectomy, which disclosed a large submacular hemorrhage with chronical features and disciform scarring in the setting of neovascular AMD.
Imaging device: Intraoperative fundus photograph
Condition/keywords: neovascular age-related macular degeneration (AMD), submacular hemorrhage, wet age-related macular degeneration (wet AMD)
-
CMV-Macula
Feb 24 2014 by Susanna S. Park, MD, PhD
Fundus photograph of a 59-year-old woman on chemotherapy for acute lymphocytic leukemia with new vision loss from cytomegalovirus retinitis
Photographer: Ellen Redenbo, UC Davis Eye Center
Condition/keywords: acute leukemia, CMV retinitis
-
 Endophthalmitis
Endophthalmitis
Feb 17 2018 by JEFFERSON R SOUSA, Tecg.º (Biomedical Systems Technology)
A 56-year-old male patient, with vision loss, with no light perception in the right eye, the presence of secretion in the anterior chamber was evaluated.
Photographer: JEFFERSON R SOUSA - Study Center and Ophthalmological Research Dr. Andre M V Gomes, Institute Dr. Suel Abujamra São Paulo-Brazil
Imaging device: Topcon TRC-50 DX, Imaginet 5.0, angle de 35 graus. Flash 36, image with digital zoom.
Condition/keywords: endophthalmitis
-
 Example of AREDS Category 1 (Small Drusen But Not Considered AMD)
Example of AREDS Category 1 (Small Drusen But Not Considered AMD)
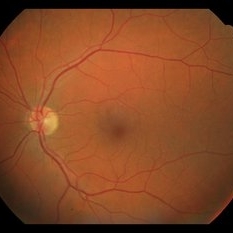
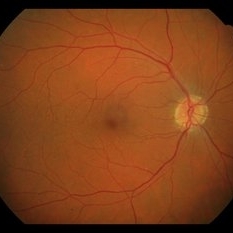
Feb 11 2013 by Neil M. Bressler, MD
Person in AREDS Category 1 were essentially free of age-related macular abnormalities, with a total drusen area less than 5 small drusen (<63 microns) within 3,000 microns of the center of the macula, and visual acuity of 20/32 or better in both eyes1. These are fundus photographs of a 53-year-old man, with visual acuity 20/20 OD and 20/32 OS presenting for evaluation of any diabetic retinopathy. Reference: 1 Age-Related Eye Disease Study Research Group. A randomized, placebo controlled clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report No. 8. Arch Ophthalmol. 2001;119(10):1417-1436.
Condition/keywords: age-related macular degeneration (AMD)
-
 Example of AREDS Category 1 (Small Drusen But Not Considered AMD)
Example of AREDS Category 1 (Small Drusen But Not Considered AMD)
Feb 11 2013 by Neil M. Bressler, MD
Person in AREDS Category 1 were essentially free of age-related macular abnormalities, with a total drusen area less than 5 small drusen (<63 microns) within 3,000 microns of the center of the macula, and visual acuity of 20/32 or better in both eyes1. These are fundus photographs of a 53-year-old man, with visual acuity 20/20 OD and 20/32 OS presenting for evaluation of any diabetic retinopathy. Reference: 1 Age-Related Eye Disease Study Research Group. A randomized, placebo controlled clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report No. 8. Arch Ophthalmol. 2001;119(10):1417-1436.
Condition/keywords: age-related macular degeneration (AMD)
-
 Gyrate Atrophy
Gyrate Atrophy
Oct 31 2018 by Dhaivat Shah
50-year-old male came in with complaint of daytime vision loss for a year and nighttime vision loss for more than 20 years, gradually increasing day by day. Fundus showed paving-stone like areas of atrophy of the RPE involving the macula which coalesces to form a characteristic scalloped border at the junction of normal and abnormal RPE. Gyrate atrophy is an autosomal recessive dystrophy caused by tenfold elevations of plasma ornithine, which is toxic to the RPE and choroid. Patients with gyrate atrophy have hyperpigmented fundi, with lobular loss of the RPE and choroid, normally sparing the fovea. The finding of generalized hyperpigmentation of the remaining RPE helps to clinically distinguish gyrate atrophy from choroideremia. Affected patients usually develop night blindness during the first decade of life and experience progressive loss of visual field and visual acuity later in the disease course. Early diagnosis is crucial because treatment in form of Arginine free diet and oral pyridoxine helps in slowing the progression of disease.
Imaging device: Optos
Condition/keywords: fundus autofluorescence (FAF), gyrate atrophy
-
---thumb.jpg/image-square;max$300,300.ImageHandler) Harada's with Exudative RD
Harada's with Exudative RD
Oct 13 2012 by Edwin H. Ryan, MD
OCT of a 35-year-old woman with acute vision loss in one eye.
Condition/keywords: exudative retinal detachment, Harada's disease
-
 Hemorrhagic Retinal Arterial Macroaneurysm
Hemorrhagic Retinal Arterial Macroaneurysm
Jul 4 2025 by Julian Navarro Saucedo
Fundus photograph of a 52-year-old woman with sudden vision loss showing a hemorrhagic retinal arterial macroaneurysm.
Photographer: Julian Navarro, Tecnologico de Monterrey, Escuela de Medician y Ciencias de la Salud.
Imaging device: VISUCAM 524 ZEISS
Condition/keywords: macroaneurysm
-
 MIDD (Maternally Inherited Diabetes and Deafness) - Left AF
MIDD (Maternally Inherited Diabetes and Deafness) - Left AF
Nov 30 2024 by John S. King, MD
Both right and left eyes have symmetrical ring of mottled hypo/hyper AF around the fovea and disc. The HyperAF areas correspond to RPE deposits on OCT as well as areas of blockage on FA, and drusenoid deposits seen on fundus photos 57 yo WF referred for AMD vs Pattern Dystrophy that was diagnosed 10 years ago. Reported some slow progressive vision loss in both eyes for distance and near. Denies nyctalopia or hemeralopia. Background medical history includes HTN, CVD, and DM. No family history of eye problems. Denied pentosan use. Anterior segment showed moderate cataracts (OD>OS). Posterior segment exam showed macular changes and mild NPDR. The macular appearance showed a symmetrical, paramacular ring of fleck-like drusenoid material with some faint focal areas of RPE hyperplasia. Fundus Photos, AF, OCT were performed as well as a gene test. Further questioning showed revealed that her mother and maternal grandmother had both diabetes mellitus and sensorineural hearing loss. The patient developed diabetes in her teens, and some high frequency hearing loss in her early twenties. She had not had a previous genetic test or diagnosis of MIDD. Gene testing is pending for the mitochondrial component. Invitae's retinal panel, which does not include mitochondrial disorders, only showed a variant of uncertain significance, HMCN1. I discussed this case with Dr. Freund, and it is similar to a the case report : Inoue M, Kiss S, Freund KB. MACULAR PIGMENT RINGS AS THE PRESENTING FINDING OF MITOCHONDRIAL MYOPATHY, ENCEPHALOPATHY, LACTIC ACIDOSIS, AND STROKELIKE EPISODES. Retin Cases Brief Rep. 2015 Fall;9(4):260-4. doi: 10.1097/ICB.0000000000000182. PMID: 26200388.
Photographer: Grace Melton and Carley Gunn
Imaging device: Clarus
Condition/keywords: Macular Dystrophy, Maternally Inherited Diabetes and Deafness, MIDD, Mitochondrial Disorder
-
 Mild Patton's Lines in IIH - Initial Photos
Mild Patton's Lines in IIH - Initial Photos
Jan 16 2019 by John S. King, MD
18-year-old African American female with increased BMI with a history of headaches, nausea, transient diplopia and vision loss that she notices when getting up from her bed (and goes away after standing upright) for the last two weeks. Went to PCP and was treated for the flu, and after no improvement and visual symptoms known, was sent to ED. MRI did not show any masses and showed empty sella turcia. Vision 20/30 OD and 20/20 OS; no RAPD; IOP 15OU; no anterior segment or vitreous inflammation; discs are elevated with obscuration of the disc margins and some of the smaller vessels; there are no SVPs; there are mild Patton's lines temporally (see Initial Photos). The optic disc cube shows 360 degrees of RNFL thickening (see OCT). Was referred to near-ophthalmologist, Dr. Doyle. She obtained additional work-up, and LP opening pressure was high, and MRV showed bilateral transverse sinus stenosis. Patient showed steady improvement with medical therapy, that included weight loss and oral diamox. On her last visit with Dr. Doyle, vision has remained stable at 20/20-20/25 without an enlarged blindspot; there are SVPs and optic disc edema has resolved (see Post Treatment Photos); she is currently on 1000 mg of diamox and has lost 15 pounds, and no stinting procedure needed.
Photographer: Gretchen Harper
Imaging device: Topcon 50
Condition/keywords: idiopathic intracranial hypertension, optic disc edema, papilledema, Patton's Lines
-
 Moyamoya: FA 2 Min OD of an Acute CRAO with CRA Sparing
Moyamoya: FA 2 Min OD of an Acute CRAO with CRA Sparing
Nov 17 2019 by John S. King, MD
60-year-old white female presented with five days of acute vision loss in the right eye. She was seen initially by referring doctor after hours five days ago and diagnosed with a CRAO and sent to ED to be evaluated stroke team. Right ICA was 100% closed but completely bypassed. She called four days later c/o redness and eye pain; at this point prominent iris vessels were seen, and she was sent to us. Her background history includes a diagnosis of moyamoya (underwent bilateral cerebral artery bypass 2015); atorvastatin for hypercholesterolemia; ASA; no hx of HTN or heart disease. She had a scleral buckle repair OD in 2017 and later developed a thick ERM, which was repaired in 2018; on her previous visit her acuity was noted at 20/40. On presentation her visual acuity was HM OD and 20/15 OS. IOP was 8 OD and 10 OS. There were prominent iris vessels in the right eye, no cell or flare, and an IOL. The posterior segment exam showed diffuse retinal whitening with attenuated vessels and boxcarring; there was sparing retinal whitening in a central area of the macula that appeared to be supplied by a cilio-retina artery. The FA showed very slow filling of the retinal vessels; there was some early perfusion secondary to the cilio-retinal artery. At 7 minutes there was still significant areas of non-perfusion, as well as macular ischemia. Avastin was administered, and one week later, PRP was performed. On the day PRP was performed, the irregular iris vessels had regressed completely. She said that she had a "sliver" of vision centrally in that eye; her acuity was CF 2' and IOP 12.
Photographer: Gretchen Harper
Imaging device: Topcon
Condition/keywords: central retinal artery occlusion (CRAO), cilioretinal sparing, moyamoya, neovascularization of iris (NVI)

 Loading…
Loading…