Search results (54 results)
-
 Suspicious Lesion 18 Years s/p Iris Resection
Suspicious Lesion 18 Years s/p Iris Resection
Oct 15 2024 by Virginia Gebhart
85 year old female with small pigmented lesion present s/p sectoral iridectomy in 2006. Lesion is suspicious for recurrence of melanoma after 18 years. Stable compared to previous exam in March 2024, unclear if this is a new lesion or has been present for an extended time. Will monitor closely.
Photographer: Virginia Gebhart, Retina Consultants of Carolina
Imaging device: Samsung Galaxy
Condition/keywords: iris melanoma, melanoma
-
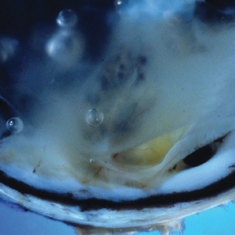
 Recurrence of Ocular Toxoplasmosis
Recurrence of Ocular Toxoplasmosis
Apr 11 2022 by Aniruddha K Agarwal, MD
Inactive toxoplasmosis lesion with active lesion at the inferior edge. The active lesion appears "fuzzy". Note also the overlying vitritis
Photographer: Debra A. Goldstein, MD, FRCSC Magerstadt Professor of Ophthalmology Director, Uveitis Service Director, Uveitis Fellowship Department of Ophthalmology Northwestern University Feinberg School of Medicine
Condition/keywords: IUSG, recurrence, retinochoroiditis, toxoplasmosis chorioretinitis, uveitis
-
 Subretinal Fibrosis and Uveitis Syndrome
Subretinal Fibrosis and Uveitis Syndrome
May 18 2020 by McGill University Health Centre
Uveitis syndrome is a rare posterior uveitis that usually begins as a multifocal choroiditis and then progresses to subretinal fibrosis. Recurrences are not uncommon and the visual prognosis is generally poor. In this enucleation specimen, a thickened choroid is clearly observed (arrow). The retina is detached and a fibrovascular subretinal membrane is present (arrowhead).
Condition/keywords: subretinal fibrosis, uveitis
-
 Choroidal Hemangioma: OCT One Month (L) and Two Months (R) Since PDT
Choroidal Hemangioma: OCT One Month (L) and Two Months (R) Since PDT
Nov 17 2019 by John S. King, MD
67-year-old white male with 6 days of decreased vision and known history of choroidal hemangioma, who had received PDT years ago for symptomatic SRF, had recurrence of SRF. PDT was applied to the lesion and one month later there is less subfoveal SRF, and vision has increased to 20/50 from 20/150. One month later the OCT shows that SRF continues to decrease and vision has improved to 20/40.
Condition/keywords: choroidal hemangioma
-
 SRF Before and Shortly After PDT for Circumscribed Choroidal Hemangioma
SRF Before and Shortly After PDT for Circumscribed Choroidal Hemangioma
Oct 12 2019 by John S. King, MD
67-year-old white male with 6 days of decreased vision and known history of choroidal hemangioma, who had received PDT years ago for symptomatic SRF, had recurrence of SRF. PDT was applied to the lesion and one month later there is less subfoveal SRF (see image), and vision has increased to 20/50 from 20/150. Will follow up in a month.
Photographer: Shelly Blair
Condition/keywords: choroidal hemangioma, photodynamic therapy
-
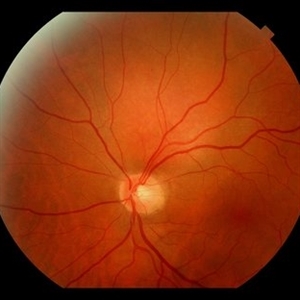 Circumscribed Choroidal Hemangioma
Circumscribed Choroidal Hemangioma
Oct 12 2019 by John S. King, MD
67-year-old white male with 6 days of decreased vision and known history of choroidal hemangioma, who had received PDT years ago for symptomatic SRF, had recurrence of SRF. PDT was applied to the lesion and one month later there is less subfoveal SRF, and vision has increased to 20/50 from 20/150. Will follow up in a month. Pictured is an orange-red choroidal mass with margins that blend with the surrounding choroid.
Photographer: Shelly Blair
Condition/keywords: choroidal hemangioma, photodynamic therapy
-
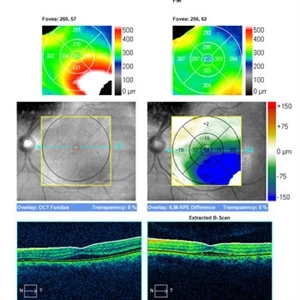
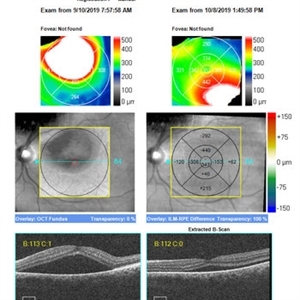
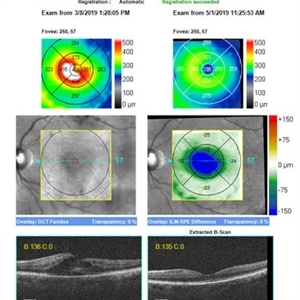 Fingolimob Associated Macular Edema (FAME)?
Fingolimob Associated Macular Edema (FAME)?
Jun 1 2019 by John S. King, MD
60 year old caucasian female with two week history of decreased vision in the left eye. Background history includes multiple sclerosis for which she uses Gileyna for the past five years, and no history of uveitis or recent MS relapse. Her vision in the left eye was 20/100 J5. The eye appeared overall "quiet" with the exception of rare cells in the anterior vitreous. The fundus appearance and FA can be seen in the images provided. OCT shows CME and SRF in OS only (left image). STK was administered and neurologist was able to discontinue the Gileyna. STK has been reported to be effective in FAME in patients who continue Gileyna (see below). 10 days later the CME had decreased significantly. 8 weeks later the edema had resolved as seen in the OCT images of the initial and latest appearance. Of note, this is a late presentation for FAME, and there was some rare debris in the anterior vitreous; it is possible, although no history of uveitis and the MS was inactive, that the CME may be related to other causes like uveitis (if there is recurrence of CME while patient is off Gileyna, then further work-up will be performed) Minuk A, Belliveau MJ, Almeida DR, Dorrepaal SJ, Gale JS. Fingolimod-associated macular edema: resolution by sub-tenon injection of triamcinolone with continued fingolimod use. JAMA ophthalmol 2013; 131(6): 802–804.
Photographer: Kay Dalby
Imaging device: Cirrus
Condition/keywords: cystoid macular edema (CME), Gilenya, macular edema
-
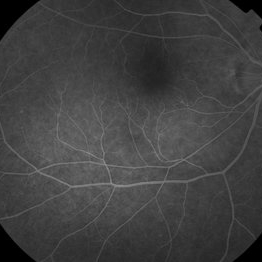
 Recurrent Subfoveal CNVM
Recurrent Subfoveal CNVM
Mar 26 2019 by Gary R. Cook, MD, FACS
63-year-old white male with exudative AMD and a subfoveal CNV 6 weeks after Argon laser photocoagulation OS per MPS Protocol for subfoveal treatment; VA decreased to 20/100.
Imaging device: Topcon VT-50
Condition/keywords: neovascular age-related macular degeneration (AMD), subfoveal choroidal neovascularization, subretinal neovascularization (SRNV), treated recurrence
-
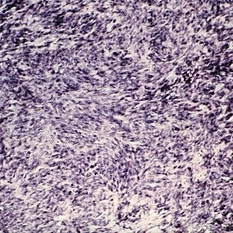 Slide 6-28
Slide 6-28
Mar 20 2019 by Lancaster Course in Ophthalmology
Fibrosarcoma. Recurrence 3 years later is highly cellular and contains many mitotic figures (H&E x80).
Condition/keywords: fibrosarcoma
-
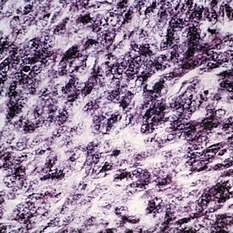 Slide 6-29
Slide 6-29
Feb 25 2019 by Lancaster Course in Ophthalmology
Fibrosarcoma. Recurrence at higher magnification (H&E x300).
Condition/keywords: fibrosarcoma
-
 Acute Posterior Multifocal Placoid Pigment Epitheliopathy
Acute Posterior Multifocal Placoid Pigment Epitheliopathy
Jan 4 2019 by Cláudia Farinha
Composite image of both eyes of a 27-year-old male with APMPPE. In the fundus photograph, multiple yellowish placoid lesions are observed in the posterior pole in both eyes. The ICGA revealed more lesions than those observed in fundoscopy, and these were hypofluorescent through the angiogram as expected. The en face OCTA segmented at the level of the choriocapillaris revealed areas of ischemia in close correspondence with the hypofluorescent lesions (image superimposed in ICGA ). The OCT b-scan with superimposed flow shows disruption and hyperreflectivity of the external retinal layers in the affected areas and again the absence of flow in the choriocapillaris underneath. A systemic study was carried out to exclude other inflammatory and infectious causes of placoid retinochoroidopathy. The clinical picture resolved after approximately one month from the onset, without recurrence.
Photographer: Pedro Melo, Ophthalmology Department, Centro Hospitalar e Universitário de Coimbra, Coimbra Portugal
Condition/keywords: acute posterior multifocal placoid pigment epitheliopathy (APMPPE), white dot syndrome
-
 Susac's Syndrome
Susac's Syndrome
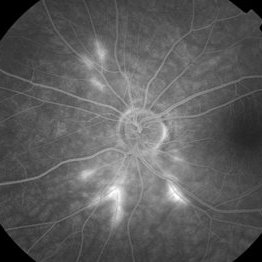
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and superotemporal BRAO OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG (this FA is one month post recurrence with resolved inferotemporal BRAO after prednisone taper and increase in IMT). She is stable and doing well with 20/20 vision in both eyes.
Photographer: Kay Dalby
Imaging device: Topcon
Condition/keywords: retinal vasculitis, Susac's syndrome
-
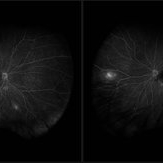 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG (FA shows a recurrence/worsening while adjusting IMT). She is stable and doing well with 20/20 vision in both eyes.
Photographer: Macey Highfill
Imaging device: Topcon
Condition/keywords: retinal vasculitis, Susac's syndrome
-
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG (FA shows a recurrence/worsening while adjusting IMT). She is stable and doing well with 20/20 vision in both eyes.
Photographer: Kay Dalby
Imaging device: Topcon
Condition/keywords: retinal vasculitis, Susac's syndrome
-
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG (FA shows a recurrence/worsening while adjusting IMT). She is stable and doing well with 20/20 vision in both eyes.
Photographer: Kay Dalby
Imaging device: Topcon
Condition/keywords: retinal vasculitis, Susac's syndrome
-
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG Background: 46yo WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG (FA shows a recurrence/worsening while adjusting IMT). She is stable and doing well with 20/20 vision in both eyes.
Photographer: Kay Dalby
Imaging device: Topcon
Condition/keywords: retinal vasculitis, Susac's syndrome
-
 Ocular Toxoplasmosis
Ocular Toxoplasmosis
May 26 2016 by Sam Kanavati
A blue autofluorescence image of an inactive well-demarcated chorioretinal scar involving the right optic nerve head secondary to ocular toxoplasmosis in a 65 year-old female patient. This scar dates back to 1971 without any recurrence. Although the scar is extensive, visual acuity was 6/6 but with a corresponding visual field defect.
Photographer: Sam Kanavati, University Hospital Southampton NHS Foundation Trust, UK
Imaging device: Heidelberg Spectralis
Condition/keywords: inactive toxoplasmosis
-
Choroidal Metastasis
Apr 22 2016 by Mallika Goyal, MD
Left fundus of a 65-year-old male physician, ex-smoker, shows a recurrent choroidal metastasis superior to macula from primary lung carcinoma non-responsive to chemotherapy. The lesion had initially resolved with radiotherapy with recurrence at same site after 2 months.
Photographer: Mallika Goyal, MD, Apollo Health City, Hyderabad, India
Condition/keywords: choroidal metastasis
-
Choroidal Metastasis
Apr 22 2016 by Mallika Goyal, MD
Left fundus of a 65-year-old male physician, ex-smoker, shows a recurrent choroidal metastasis superior to macula from primary lung carcinoma non-responsive to chemotherapy. The lesion had initially resolved with radiotherapy with recurrence at same site after 2 months.
Photographer: Mallika Goyal, MD, Apollo Health City, Hyderabad, India
Condition/keywords: choroidal metastasis
-
Choroidal Metastasis
Apr 22 2016 by Mallika Goyal, MD
Left fundus of a 65-year-old male physician, ex-smoker, shows a recurrent choroidal metastasis superior to macula from primary lung carcinoma non-responsive to chemotherapy. The lesion had initially resolved with radiotherapy with recurrence at same site after 2 months.
Photographer: Mallika Goyal, MD, Apollo Health City, Hyderabad, India
Condition/keywords: choroidal metastasis
-
Choroidal Metastasis
Apr 22 2016 by Mallika Goyal, MD
Right fundus of a 65-year-old male physician, ex-smoker, shows a choroidal metastasis nasal to disc from primary lung carcinoma non-responsive to chemotherapy. Resolved with radiotherapy with recurrence at same site after 2 months.
Photographer: Mallika Goyal, MD, Apollo Health City, Hyderabad, India
Condition/keywords: choroidal metastasis
-
Choroidal Metastasis
Apr 22 2016 by Mallika Goyal, MD
Left fundus of a 65-year-old male physician, ex-smoker, shows a choroidal metastasis superior to macula from primary lung carcinoma non-responsive to chemotherapy. Resolved with radiotherapy with recurrence at same site after 2 months.
Photographer: Mallika Goyal, MD, Apollo Health City, Hyderabad, India
Condition/keywords: choroidal metastasis
-
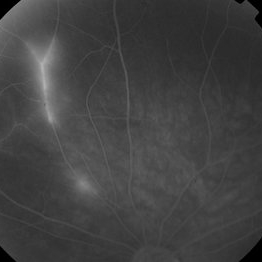
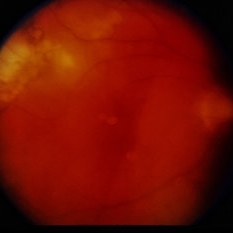 Toxoplasmosis Chorioretinitis Recurrence
Toxoplasmosis Chorioretinitis Recurrence
Oct 30 2015 by David Callanan, MD
36-year-old male, toxoplasmosis chorioretinitis recurrence.
Condition/keywords: recurrence, toxoplasmosis
-
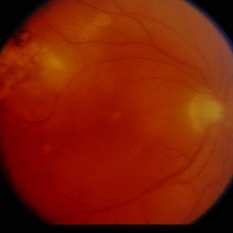 Toxoplasmosis Chorioretinitis Recurrence
Toxoplasmosis Chorioretinitis Recurrence
Oct 30 2015 by David Callanan, MD
36-year-old male, toxoplasmosis chorioretinitis recurrence.
Condition/keywords: recurrence, toxoplasmosis
-
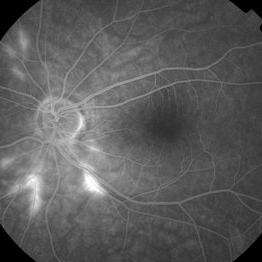
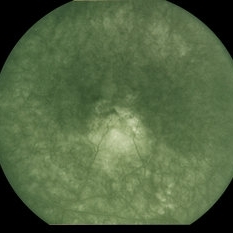 Presumed Ocular Histoplasmosis Syndrome
Presumed Ocular Histoplasmosis Syndrome
Jan 5 2015 by H. Michael Lambert, MD
Fluorescein angiogram showing subretinal new vessel membrane in foveal area, probable recurrence from previous laser.
Condition/keywords: presumed ocular histoplasmosis syndrome (POHS)

 Loading…
Loading…