Search results (2800 results)
-
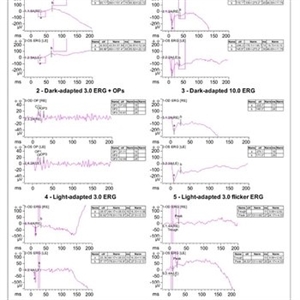 CSNB-ERG
CSNB-ERG
Aug 23 2021 by Jennifer Carstens
Full-field ERG showing electronegative B wave in patient with CACNA1F confirmed X-linked CSNB.
Photographer: Jing Zhang, Ophthalmic Photographer
Condition/keywords: CACNA1F, ERG, X-linked CSNB
-
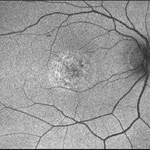
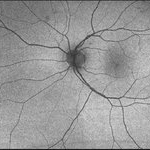
 PPCRA
PPCRA
Jan 31 2024 by Pallavi Goel
A 14-year-old male, presented to our clinic for a regular ophthalmic examination. Both Eyes Best Corrected Visual Acuity was 6/6, N6. The Indirect Ophthalmoscopic examination revealed an incidental finding in both eyes with patches of chorioretinal atrophy and pigment clumps along the veins consistent with pigmented paravenous chorioretinal atrophy (PPCRA) with early attenuation of retinal vessels, normal discs, and macula. ERG was normal. The patient was counseled and explained the nature of his condition. He was asked to be in yearly follow-up.
Photographer: Pallavi Goel, Dr. Shroff's Charity eye hospital,Delhi
Condition/keywords: ERG
-
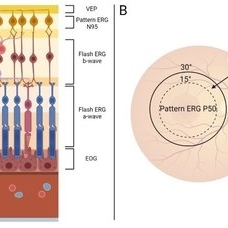 Summary of Retinal Origins of Various Electroretinographic Components
Summary of Retinal Origins of Various Electroretinographic Components
May 13 2024 by Gabrielle Hallai
Each layer of the retina can be assessed using various electroretinographic techniques. A) A summary of the retinal origins of each response is shown here. B) Macular function can be assessed by pattern and multifocal ERG recording and provide a specific assessment of central vision, while flash tests are dominated by the more peripheral retina.
Photographer: Gabrielle Hallai, PhD, Cleveland Clinic Cole Eye Institute
Condition/keywords: electroretinography, ERG
-
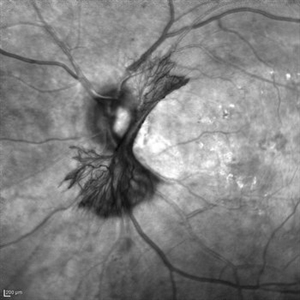 "NVD Flower"
"NVD Flower"
Oct 20 2023 by Daniel Davis, OCT-C
Infrared image of NVD (52F)
Imaging device: Heidelberg Spectralis
Condition/keywords: neovascularization of the disc (NVD)
-
---thumb.jpg/image-square;max$300,300.ImageHandler) "Solarization"
"Solarization"
Feb 20 2013 by From the Collections of Thomas M. Aaberg, MD and Thomas M. Aaberg Jr., MD
FA "eradic response to premature sxposure to room light;" extensive vascular occlusions.
Condition/keywords: solarization, vascular occlusions
-
---thumb.jpg/image-square;max$300,300.ImageHandler) "Solarization"
"Solarization"
Feb 20 2013 by From the Collections of Thomas M. Aaberg, MD and Thomas M. Aaberg Jr., MD
FA "eradic response to premature sxposure to room light."
Condition/keywords: solarization, vascular occlusions
-
 "The Eye of Sauron"
"The Eye of Sauron"
Mar 14 2023 by Anfisa Ayalon, MD
Fundus autofluorescence image of a 38-year-old female with “Bull's eye” pattern maculopathy. There is no history of medication use associated with retinal toxicity. BCVA RE 20/25+2
Photographer: Danielle Ferguson and Alec Bertoni, University of Pittsburgh Medical Center
Condition/keywords: bull's eye maculopathy, retina
-
 "Untouched" Intra-ocular Foreign Body - Course Over 7 Years!
"Untouched" Intra-ocular Foreign Body - Course Over 7 Years!
Jul 7 2020 by Deependra Vikram Singh, MD FASRS
25-yr-old male presented to our retina clinic in 2007 with history of Hammer and chisel injury to left eye 2 months back. On examination BCVA in left eye was 20/20. Slit-lamp examination revealed iris hole and fundus examination showed an encapsulated metallic intraocular foreign body (IOFB) close to inferior arcade in left eye. Patient was advised Vitreous surgery with IOFB removal. Patient, however did not turn up for Surgery and revisited our clinic after seven years in 2014. On examination his BCVA was 20/20 in left eye and IOFB has reduced in size with brown siderotic deposits seen over IOFB capsule. Examination revealed posterior sub-capsular cataract but no siderotic changes with intraocular pressure (IOP) also being recorded as normal. In view of good visual acuity and no siderotic changes, he was advised regular follow up and ERG. Since most IOFBs would get timely removed by vitreous surgery, this Image capturing the natural course of a metallic IOFB is rare.
Photographer: Deependra Vikram Singh, Eye-Q Hospitals, Gurugram, INDIA
Imaging device: Kowa and Zeiss
Condition/keywords: encapsulated intraocular foreign body
-
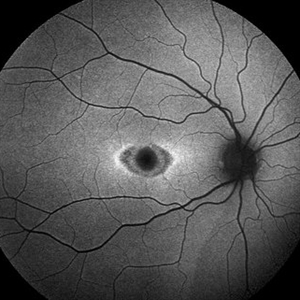
 “Bull's eye” pattern maculopathy
“Bull's eye” pattern maculopathy
Mar 14 2023 by Anfisa Ayalon, MD
Left eye fundus autofluorescence image of a 38-year-old female with “Bull's eye” pattern maculopathy. There is no history of medication use associated with retinal toxicity. BCVA LE 20/20-3
Photographer: Danielle Ferguson and Alec Bertoni, University of Pittsburgh Medical Center
Condition/keywords: bull's eye maculopathy, Maculopathy, retina
-
 01 Unilateral Acute Idiopathic Maculopathy (UAIM) Pseudocolor Photograph OD
01 Unilateral Acute Idiopathic Maculopathy (UAIM) Pseudocolor Photograph OD
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of pt's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, patient mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT , diagnosed with CSCR and referred for retina evaluation. - ROS/ PMHx: negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - pseudocolor and FAF photos: RPE changes/ clumps with GA and stippled autofluorescense OD, unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, subfoveal ellipsoid zone atrophy with intact ELM with no CME or SRF OD, unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG and VF - patient rescheduled
Imaging device: Optos - California
Condition/keywords: unilateral acute idiopathic maculopathy
-
 02 Unilateral Acute Idiopathic Maculopathy (UAIM) - Pseudocolor Photograph OS
02 Unilateral Acute Idiopathic Maculopathy (UAIM) - Pseudocolor Photograph OS
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of pt's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, pt mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT , diagnosed with CSCR and referred for retina evaluation. - ROS/ PMHx: Negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - Pseudocolor and FAF photos: RPE changes/ clumps w/ GA and stippled autofluorescense OD, unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, Subfoveal ellipsoid zone atrophy w/ intact ELM W/No CME or SRF OD, Unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG & VF - patient rescheduled
Imaging device: Optos - California
Condition/keywords: unilateral acute idiopathic maculopathy
-
 03- Unilateral Acute Idiopathic Maculopathy (UAIM) - FAF OD
03- Unilateral Acute Idiopathic Maculopathy (UAIM) - FAF OD
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of patient's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, pt mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT , diagnosed w/ CSCR and referred for retina evaluation. - ROS/ PMHx: Negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - Pseudocolor & FAF photos: RPE changes/ clumps with GA and stippled autofluorescense OD, Unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, subfoveal ellipsoid zone atrophy with intact ELM with no CME or SRF OD, unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG & VF - pt rescheduled!
Imaging device: Optos - California
Condition/keywords: unilateral acute idiopathic maculopathy
-
 04- Unilateral Acute Idiopathic Maculopathy (UAIM) - FAF OS
04- Unilateral Acute Idiopathic Maculopathy (UAIM) - FAF OS
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of pateint's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, patient mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT, diagnosed with CSCR and referred for retina evaluation. - ROS/ PMHx: negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - pseudocolor and FAF photos: RPE changes/ clumps with GA & stippled autofluorescence OD, unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, subfoveal ellipsoid zone atrophy with intact ELM with no CME or SRF OD, unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG & VF - patient rescheduled
Imaging device: Optos - California
Condition/keywords: unilateral acute idiopathic maculopathy
-
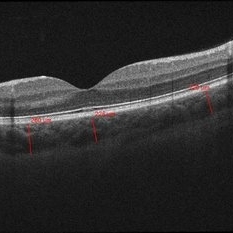
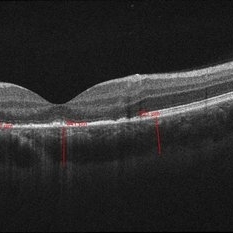 05- Unilateral Acute Idiopathic Maculopathy (UAIM) - OCT OD
05- Unilateral Acute Idiopathic Maculopathy (UAIM) - OCT OD
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of pt's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, pt mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT , diagnosed with CSCR and referred for retina evaluation. - ROS/ PMHx: Negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - Pseudocolor and FAF photos: RPE changes/ clumps w/ GA and stippled autofluorescense OD, unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, Subfoveal ellipsoid zone atrophy w/ intact ELM W/No CME or SRF OD, Unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG & VF - patient rescheduled
Imaging device: Zeiss-Cirrus 4000
Condition/keywords: unilateral acute idiopathic maculopathy
-
 05- Unilateral Acute Idiopathic Maculopathy (UAIM) - OCT OD2
05- Unilateral Acute Idiopathic Maculopathy (UAIM) - OCT OD2
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of pt's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, pt mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT , diagnosed with CSCR and referred for retina evaluation. - ROS/ PMHx: Negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - Pseudocolor and FAF photos: RPE changes/ clumps w/ GA and stippled autofluorescense OD, unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, Subfoveal ellipsoid zone atrophy w/ intact ELM W/No CME or SRF OD, Unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG & VF - patient rescheduled
Imaging device: Zeiss-Cirrus 4000
Condition/keywords: unilateral acute idiopathic maculopathy
-
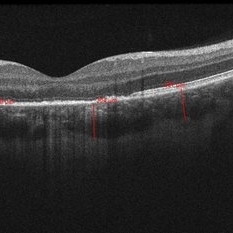
 06- Unilateral Acute Idiopathic Maculopathy (UAIM) - OCT OS
06- Unilateral Acute Idiopathic Maculopathy (UAIM) - OCT OS
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of pt's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, pt mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT , diagnosed with CSCR and referred for retina evaluation. - ROS/ PMHx: Negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - Pseudocolor and FAF photos: RPE changes/ clumps w/ GA and stippled autofluorescense OD, unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, Subfoveal ellipsoid zone atrophy w/ intact ELM W/No CME or SRF OD, Unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG & VF - patient rescheduled
Imaging device: Zeiss-Cirrus 4000
Condition/keywords: unilateral acute idiopathic maculopathy
-
---thumb.jpg/image-square;max$300,300.ImageHandler) Abnormal Fundus
Abnormal Fundus
Oct 15 2013 by Maurice F. Rabb
The patient is a 48 year old female who was noted to have an abnormal fundus on routine examination. Her past medical history is unremarkable. Her past family history is remarkable for her father being diagnosed with macular degeneration at age 72. Visual acuity was 20/20-1, J-2, OD and 20/20, J-1, OS. Amsler grid examinaton was normal, OU. All 6 of the AOHRR screening plates were identified correctly, OU. The 45 minute rod psychophysiologic threshold was normal, OU. ERG responses were normal for both rod and cone amplitudes. The cone implicit times were normal. The EOG was normal.
Condition/keywords: abnormal fundus
-
---thumb.jpg/image-square;max$300,300.ImageHandler) Abnormal Fundus
Abnormal Fundus
Oct 15 2013 by Maurice F. Rabb
The patient is a 48 year old female who was noted to have an abnormal fundus on routine examination. Her past medical history is unremarkable. Her past family history is remarkable for her father being diagnosed with macular degeneration at age 72. Visual acuity was 20/20-1, J-2, OD and 20/20, J-1, OS. Amsler grid examinaton was normal, OU. All 6 of the AOHRR screening plates were identified correctly, OU. The 45 minute rod psychophysiologic threshold was normal, OU. ERG responses were normal for both rod and cone amplitudes. The cone implicit times were normal. The EOG was normal.
Condition/keywords: abnormal fundus
-
---thumb.jpg/image-square;max$300,300.ImageHandler) Abnormal Fundus
Abnormal Fundus
Oct 15 2013 by Maurice F. Rabb
The patient is a 48 year old female who was noted to have an abnormal fundus on routine examination. Her past medical history is unremarkable. Her past family history is remarkable for her father being diagnosed with macular degeneration at age 72. Visual acuity was 20/20-1, J-2, OD and 20/20, J-1, OS. Amsler grid examinaton was normal, OU. All 6 of the AOHRR screening plates were identified correctly, OU. The 45 minute rod psychophysiologic threshold was normal, OU. ERG responses were normal for both rod and cone amplitudes. The cone implicit times were normal. The EOG was normal.
Condition/keywords: abnormal fundus
-
---thumb.jpg/image-square;max$300,300.ImageHandler) Abnormal Fundus
Abnormal Fundus
Oct 15 2013 by Maurice F. Rabb
The patient is a 48 year old female who was noted to have an abnormal fundus on routine examination. Her past medical history is unremarkable. Her past family history is remarkable for her father being diagnosed with macular degeneration at age 72. Visual acuity was 20/20-1, J-2, OD and 20/20, J-1, OS. Amsler grid examinaton was normal, OU. All 6 of the AOHRR screening plates were identified correctly, OU. The 45 minute rod psychophysiologic threshold was normal, OU. ERG responses were normal for both rod and cone amplitudes. The cone implicit times were normal. The EOG was normal.
Condition/keywords: abnormal fundus
-
---thumb.jpg/image-square;max$300,300.ImageHandler) Abnormal Fundus
Abnormal Fundus
Oct 15 2013 by Maurice F. Rabb
The patient is a 48 year old female who was noted to have an abnormal fundus on routine examination. Her past medical history is unremarkable. Her past family history is remarkable for her father being diagnosed with macular degeneration at age 72. Visual acuity was 20/20-1, J-2, OD and 20/20, J-1, OS. Amsler grid examinaton was normal, OU. All 6 of the AOHRR screening plates were identified correctly, OU. The 45 minute rod psychophysiologic threshold was normal, OU. ERG responses were normal for both rod and cone amplitudes. The cone implicit times were normal. The EOG was normal.
Condition/keywords: abnormal fundus
-
---thumb.jpg/image-square;max$300,300.ImageHandler) Abnormal Fundus
Abnormal Fundus
Oct 15 2013 by Maurice F. Rabb
The patient is a 48 year old female who was noted to have an abnormal fundus on routine examination. Her past medical history is unremarkable. Her past family history is remarkable for her father being diagnosed with macular degeneration at age 72. Visual acuity was 20/20-1, J-2, OD and 20/20, J-1, OS. Amsler grid examinaton was normal, OU. All 6 of the AOHRR screening plates were identified correctly, OU. The 45 minute rod psychophysiologic threshold was normal, OU. ERG responses were normal for both rod and cone amplitudes. The cone implicit times were normal. The EOG was normal.
Condition/keywords: abnormal fundus
-
---thumb.jpg/image-square;max$300,300.ImageHandler) Abnormal Fundus
Abnormal Fundus
Oct 15 2013 by Maurice F. Rabb
The patient is a 48 year old female who was noted to have an abnormal fundus on routine examination. Her past medical history is unremarkable. Her past family history is remarkable for her father being diagnosed with macular degeneration at age 72. Visual acuity was 20/20-1, J-2, OD and 20/20, J-1, OS. Amsler grid examinaton was normal, OU. All 6 of the AOHRR screening plates were identified correctly, OU. The 45 minute rod psychophysiologic threshold was normal, OU. ERG responses were normal for both rod and cone amplitudes. The cone implicit times were normal. The EOG was normal.
Condition/keywords: abnormal fundus
-
---thumb.jpg/image-square;max$300,300.ImageHandler) Abnormal Fundus
Abnormal Fundus
Oct 15 2013 by Maurice F. Rabb
The patient is a 48 year old female who was noted to have an abnormal fundus on routine examination. Her past medical history is unremarkable. Her past family history is remarkable for her father being diagnosed with macular degeneration at age 72. Visual acuity was 20/20-1, J-2, OD and 20/20, J-1, OS. Amsler grid examinaton was normal, OU. All 6 of the AOHRR screening plates were identified correctly, OU. The 45 minute rod psychophysiologic threshold was normal, OU. ERG responses were normal for both rod and cone amplitudes. The cone implicit times were normal. The EOG was normal.
Condition/keywords: abnormal fundus
-
 Aborted Arteriolitis
Aborted Arteriolitis
Feb 15 2013 by From the Collections of Thomas M. Aaberg, MD and Thomas M. Aaberg Jr., MD
Fundus photograph showing activated toxoplasma retinochoroiditis with active retinal whitening adjacent to a hyperpigmented scar in the superonasal mid-periophery.
Condition/keywords: ocular toxoplasmosis

 Loading…
Loading…