Search results (53 results)
-
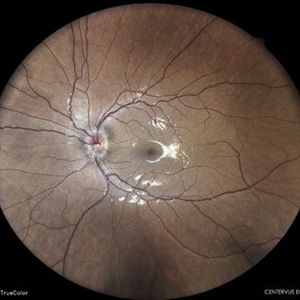
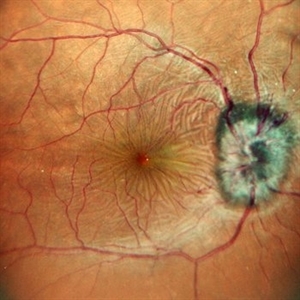
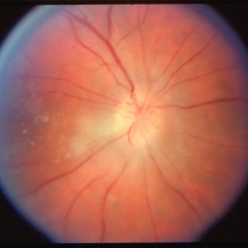
 Myelinated Nerve Fibers
Myelinated Nerve Fibers
Apr 18 2025 by DR Rohit Gupta
The **myelinated nerve fibers of the optic disc** (also known as **medullated nerve fibers**) are retinal nerve fibers that retain their myelin sheath as they pass through the optic nerve head. Normally, retinal nerve fibers are unmyelinated to allow for light transparency, but in some cases, myelination extends anteriorly into the retina, appearing as a striking white, feathery patch on the optic disc or peripapillary retina. ### **Key Features:** 1. **Appearance:** - Dense, white, striated patches with feathery edges. - Typically located at the superior or inferior pole of the optic disc. - May obscure retinal vessels underneath. 2. **Clinical Significance:** - Usually **benign** and asymptomatic. - **Congenital** (present at birth or early childhood). - Rarely associated with **visual field defects** (e.g., scotomas corresponding to the area of myelination). - Occasionally linked with **high myopia** or **amblyopia** if extensive. 3. **Pathophysiology:** - Failure of oligodendrocytes or Schwann cells to stop myelination at the lamina cribrosa. - Normally, myelination stops at the optic nerve head, but in this condition, it extends into the retina. 4. **Diagnosis:** - **Fundoscopy:** Classic white, feathery appearance. - **Optical Coherence Tomography (OCT):** Shows thickened retinal nerve fiber layer (RNFL). - **Visual Field Testing:** May detect defects if large. 5. **Differential Diagnosis:** - Optic disc edema - Cotton wool spots - Retinoblastoma (rarely, but must be ruled out in children) 6. **Management:** - No treatment required if asymptomatic. - Monitor for amblyopia in children. - Rare cases with significant visual impairment may need further evaluation. ### **Fun Fact:** Myelinated nerve fibers are seen in **~0.5-1%** of the population and are usually an incidental finding.
Photographer: Dr Rohit gupta
Imaging device: Samsung S21
Condition/keywords: Medulated Nerve fibre, Medullated Nerve fibres, myelinated nerve fibers, Myelinated Nerve Fibres, optic disc drusen
-
 Unilateral Disc Edema
Unilateral Disc Edema
May 7 2024 by Akansha Sharma
Color fundus photograph of a 27 year old male with unilateral optic disc edema.
Photographer: Dr. Akansha Sharma, Bharati Eye Hospital
Condition/keywords: disc edema, optic disc edema
-
 Disc Edema
Disc Edema
Apr 17 2024 by Akansha Sharma
Color fundus photograph of a 35 year old female with disc edema.
Photographer: Dr. Akansha Sharma, Bharati Eye Hospital
Condition/keywords: Disc Edema, optic disc edema
-
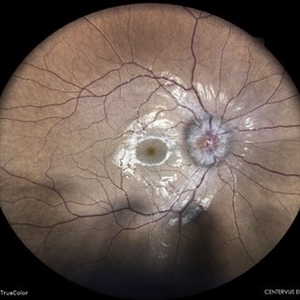
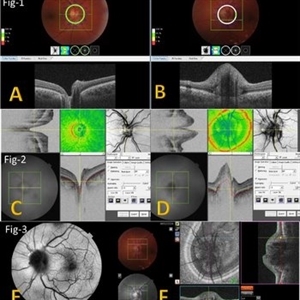 Multimodal Imaging for Differentiating Unilateral Pseudo Optic Disc Swelling(Buried Drusen) From True Optic Disc Swelling
Multimodal Imaging for Differentiating Unilateral Pseudo Optic Disc Swelling(Buried Drusen) From True Optic Disc Swelling
Feb 7 2024 by Fawwaz F Al Mamoori, MD, Medical Retina Consultant
27-year-old male, medically free, presented with left unilateral optic disc swelling. BCVA=1.0(OU), color vision, and contrast sensitivity were normal (OU)with no RAPD in the left eye. Swept Source OCT: showed elevated left optic disc with hyporeflective mass (Fig-1 B). Enface OCT: Showed left peripapillary multiple ovoid mass lesions(drusen) (Fig-2 d, Fig3 F). FAF: of the left eye showed superonasal hyper autofluorescent drusenoid lesions)(Fig3 E). Orbital MRI with contrast was requested to exclude any compressive lesions like tumors(menigioma)or inflammatory lesions like granuloma(sarcoid granuloma). orbital MRI result was normal.
Photographer: Hana.S.Owais
Imaging device: TRITON(TOPCON,Swept Source OCT)
Condition/keywords: fundus autofluorescence (FAF), multimodal imaging, OCT EN FACE, optic disc drusen, optic disc edema, swept source
-
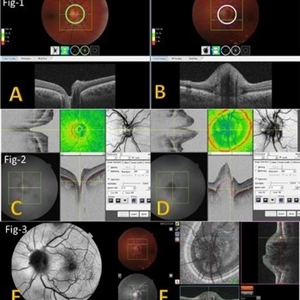 Multimodal Imaging for Differentiating Unilateral Pseudo Optic Disc Swelling(Buried Drusen) From True Optic Disc Swelling
Multimodal Imaging for Differentiating Unilateral Pseudo Optic Disc Swelling(Buried Drusen) From True Optic Disc Swelling
Feb 7 2024 by Fawwaz F Al Mamoori, MD, Medical Retina Consultant
A 27-year-old male patient, medically free, presented with unilateral left optic disc swelling. BCVA=1.0(OU), color vision, and contrast sensitivity were normal (OU) with no RAPD in the left eye. SS-OCT: showed left optic disc elevation with hyporeflective mass lesion (Fig-1 B). Enface OCT: showed left peripapillary hyperreflective ovoid mass lesions(Fig-2 D, Fig-3 F), FAF: showed left superonasal hyperautofluorescent drusenoid lesions. Orbital MRI with contrast was requested to exclude any optic nerve compressive lesions like (tumors: like mengioma or inflammatory lesions like granuloma (sarcoidosis). the result of orbital MRI was normal.
Photographer: Hana.S.Owais
Imaging device: TRITON(TOPCON,Swept Source OCT)
Condition/keywords: fundus autofluorescence (FAF), multimodal imaging, OCT EN FACE, optic disc drusen, optic disc edema
-
 Choroidal Granuloma
Choroidal Granuloma
Aug 6 2023 by AMIT NENE
Fundus photograph of 27 year old female with choroidal granuloma and disc edema treated with IVMP and oral steroids resulting in complete melt of granuloma at follow-up
Photographer: Gaurav Kamble, Isha Netralaya, Thane
Imaging device: Optos imaging
Condition/keywords: choroidal granuloma, optic disc edema
-
 Pseudo Foster Kennedy Syndrome
Pseudo Foster Kennedy Syndrome
Oct 13 2022 by Aditya S Kelkar, MS, FRCS, FASRS,FRCOphth
Colour fundus photograph of a 44-year-old man showing bilateral small discs with optic atrophy on the right eye and disc edema on the left eye resulting from consecutive NAAION in both eyes.
Photographer: Dr Sukanya Mondal, National Institute of Ophthalmology, Pune. India
Imaging device: Zeiss Clarus 500
Condition/keywords: ischemic optic neuropathy, optic atrophy, optic disc edema
-
 Hypotony Maculopathy
Hypotony Maculopathy
Jun 12 2022 by Pramod Kumar Suman, MBBS, MD
Fundus photograph of an 26-year-old male with retinal folds around the center of the fovea arranged in stellate pattern with optic disc edema.
Photographer: Pramod Kumar Suman, Retina Foundation, Ahmedabad
Condition/keywords: hypotony maculopathy
-
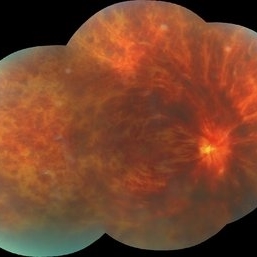 Central Retinal Vein Occlusion
Central Retinal Vein Occlusion
Nov 26 2020 by Priya Rasipuram Chandrasekaran, MBBS, DO, DNB, FRCS
A 44-year-old male patient presented with no underlying systemic illness presented with this picture showing extensive scattered superficial and deep retinal hemorrhages to confluent retinal hemorrhages extending to all the quadrants associated with marked dilatation and tortuosity of vessels and associated with optic disc edema, macular edema and retinal thickening giving the appearance of blood and thunder retina.
Condition/keywords: central retinal vein occlusion (CRVO)
-
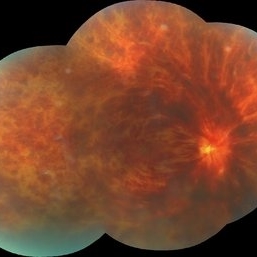
 CRVO
CRVO
Nov 26 2020 by Priya Rasipuram Chandrasekaran, MBBS, DO, DNB, FRCS
A 44-year-old male patient presented with no underlying systemic illness presented with this picture showing extensive scattered superficial and deep retinal hemorrhages to confluent retinal hemorrhages extending to all the quadrants associated with marked dilatation and tortuosity of vessels and associated with optic disc edema, macular edema and retinal thickening giving the appearance of blood and thunder retina.
Condition/keywords: central retinal vein occlusion (CRVO)
-
 Central Retinal Vein Occlusion
Central Retinal Vein Occlusion
Nov 26 2020 by Priya Rasipuram Chandrasekaran, MBBS, DO, DNB, FRCS
A 44-year-old male patient presented with no underlying systemic illness presented with this picture showing extensive scattered superficial and deep retinal hemorrhages to confluent retinal hemorrhages extending to all the quadrants associated with marked dilatation and tortuosity of vessels and associated with optic disc edema, macular edema and retinal thickening giving the appearance of blood and thunder retina.
Condition/keywords: central retinal vein occlusion (CRVO)
-
 CRVO
CRVO
Nov 26 2020 by Priya Rasipuram Chandrasekaran, MBBS, DO, DNB, FRCS
A 44-year-old male patient presented with no underlying systemic illness presented with this picture showing extensive scattered superficial and deep retinal haemorrhages to confluent retinal hemorrhages extending to all the quadrants associated with marked dilatation and tortuosity of vessels and associated with optic disc edema, macular edema and retinal thickening giving the appearance of blood and thunder retina.
Condition/keywords: central retinal vein occlusion (CRVO)
-
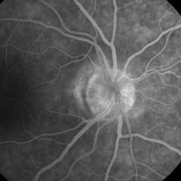 Papillophlebitis
Papillophlebitis
Dec 23 2019 by Stephanie Burke
Fluorescein angiogram, mid-phase image of a 46-year-old woman with papillophlebitis.
Photographer: Stephanie Burke, CRA, OCT-C
Imaging device: Zeiss 450 Plus
Condition/keywords: optic disc edema, papillophlebitis
-
 Disc Edema
Disc Edema
Oct 16 2019 by Prithvi Chandrakanth
26-year-old male, presented with defective vision, on examination his color vision, red desaturation test were reduced. Fundus examination revealed edematous halo around the disc suggesting progressive optic disc edema.
Photographer: Dr.Prithvi Chandrakanth, Dr.Chandrakanth Malabar Nethralaya, Kozhikode, India
Imaging device: TRASH TO TREASURE RETCAM
Condition/keywords: frisen grade 2, optic disc edema, retcam, smartphone fundus photography
-
 Post Treatment Photos: Showing Resolution of Disc Edema in Setting of IIH and Bilateral Transverse Sinus Stenosis
Post Treatment Photos: Showing Resolution of Disc Edema in Setting of IIH and Bilateral Transverse Sinus Stenosis
Jun 1 2019 by John S. King, MD
18-year-old African American female with increased BMI with a history of headaches, nausea, transient diplopia and vision loss that she notices when getting up from her bed (and goes away after standing upright) for the last two weeks. Went to PCP and was treated for the flu, and after no improvement and visual symptoms known, was sent to ED. MRI did not show any masses and showed empty sella turcia. Vision 20/30 OD and 20/20 OS; no RAPD; IOP 15OU; no anterior segment or vitreous inflammation; discs are elevated with obscuration of the disc margins and some of the smaller vessels; there are no SVPs; there are mild Patton's lines temporally (see initial photos). The optic disc cube shows 360 degrees of RNFL thickening (see OCT). Was referred to near-ophthalmologist, Dr. Doyle. She obtained additional work-up, and LP opening pressure was high, and MRV showed bilateral transverse sinus stenosis. Patient showed steady improvement with medical therapy, that included weight loss and oral diamox. On her last visit with Dr. Doyle, vision has remained stable at 20/20-20/25 without an enlarged blindspot; there are SVPs and optic disc edema has resolved (see post treatment photos); she is currently on 1000 mg of diamox and has lost 15 pounds, and no stinting procedure needed.
Condition/keywords: idiopathic intracranial hypertension, transverse sinus stenosis
-
 Post Treatment Photos: Showing Resolution of Disc Edema in Setting of IIH and Bilateral Transverse Sinus Stenosis
Post Treatment Photos: Showing Resolution of Disc Edema in Setting of IIH and Bilateral Transverse Sinus Stenosis
Jun 1 2019 by John S. King, MD
18-year-old African American female with increased BMI with a history of headaches, nausea, transient diplopia and vision loss that she notices when getting up from her bed (and goes away after standing upright) for the last two weeks. Went to PCP and was treated for the flu, and after no improvement and visual symptoms known, was sent to ED. MRI did not show any masses and showed empty sella turcia. Vision 20/30 OD and 20/20 OS; no RAPD; IOP 15OU; no anterior segment or vitreous inflammation; discs are elevated with obscuration of the disc margins and some of the smaller vessels; there are no SVPs; there are mild Patton's lines temporally (see initial photos). The optic disc cube shows 360 degrees of RNFL thickening (see OCT). Was referred to near-ophthalmologist, Dr. Doyle. She obtained additional work-up, and LP opening pressure was high, and MRV showed bilateral transverse sinus stenosis. Patient showed steady improvement with medical therapy, that included weight loss and oral diamox. On her last visit with Dr. Doyle, vision has remained stable at 20/20-20/25 without an enlarged blindspot; there are SVPs and optic disc edema has resolved (see post treatment photos); she is currently on 1000 mg of diamox and has lost 15 pounds, and no stinting procedure needed.
Condition/keywords: idiopathic intracranial hypertension, transverse sinus stenosis
-
 Papillitis and Toxoplasmosis
Papillitis and Toxoplasmosis
Apr 8 2019 by Gary R. Cook, MD, FACS
19-year-old white female with acute optic disc edema and macular exudates OD secondary to ocular toxoplasmosis; V.A. = 20/20
Condition/keywords: acute toxoplasmosis, ocular toxoplasmosis, papillitis
-
 Malignant Hypertension
Malignant Hypertension
Mar 27 2019 by Gary R. Cook, MD, FACS
Left eye of a 78-year-old Vietnamese male with malignant hypertension demonstrating ischemic optic disc edema, marked arteriolar narrowing, intraretinal hemorrhages, and lipid exudation; V.A.= counting fingers at 1 foot.
Imaging device: Topcon VT-50
Condition/keywords: hemorrhage, lipid exudation, malignant hypertension, optic disc edema
-
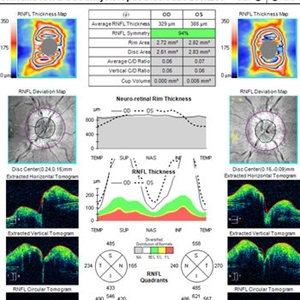 OCT in Patient With IIH Showing Thickened RNFL
OCT in Patient With IIH Showing Thickened RNFL
Jan 16 2019 by John S. King, MD
18-year-old African American female with increased BMI with a history of headaches, nausea, transient diplopia and vision loss that she notices when getting up from her bed (and goes away after standing upright) for the last two weeks. Went to PCP and was treated for the flu, and after no improvement and visual symptoms known, was sent to ED. MRI did not show any masses and showed empty sella turcia. Vision 20/30 OD and 20/20 OS; no RAPD; IOP 15OU; no anterior segment or vitreous inflammation; discs are elevated with obscuration of the disc margins and some of the smaller vessels; there are no SVPs; there are mild Patton's lines temporally (see Initial Photos). The optic disc cube shows 360 degrees of RNFL thickening (see OCT). Was referred to near-ophthalmologist, Dr. Doyle. She obtained additional work-up, and LP opening pressure was high, and MRV showed bilateral transverse sinus stenosis. Patient showed steady improvement with medical therapy, that included weight loss and oral diamox. On her last visit with Dr. Doyle, vision has remained stable at 20/20-20/25 without an enlarged blindspot; there are SVPs and optic disc edema has resolved (see Post Treatment Photos); she is currently on 1000 mg of diamox and has lost 15 pounds, and no stinting procedure needed.
Imaging device: Cirrus
Condition/keywords: benign idiopatic intracranial hypertension, optic disc edema, papilledema
-
 Mild Patton's Lines in IIH - Initial Photos
Mild Patton's Lines in IIH - Initial Photos
Jan 16 2019 by John S. King, MD
18-year-old African American female with increased BMI with a history of headaches, nausea, transient diplopia and vision loss that she notices when getting up from her bed (and goes away after standing upright) for the last two weeks. Went to PCP and was treated for the flu, and after no improvement and visual symptoms known, was sent to ED. MRI did not show any masses and showed empty sella turcia. Vision 20/30 OD and 20/20 OS; no RAPD; IOP 15OU; no anterior segment or vitreous inflammation; discs are elevated with obscuration of the disc margins and some of the smaller vessels; there are no SVPs; there are mild Patton's lines temporally (see Initial Photos). The optic disc cube shows 360 degrees of RNFL thickening (see OCT). Was referred to near-ophthalmologist, Dr. Doyle. She obtained additional work-up, and LP opening pressure was high, and MRV showed bilateral transverse sinus stenosis. Patient showed steady improvement with medical therapy, that included weight loss and oral diamox. On her last visit with Dr. Doyle, vision has remained stable at 20/20-20/25 without an enlarged blindspot; there are SVPs and optic disc edema has resolved (see Post Treatment Photos); she is currently on 1000 mg of diamox and has lost 15 pounds, and no stinting procedure needed.
Photographer: Gretchen Harper
Imaging device: Topcon 50
Condition/keywords: idiopathic intracranial hypertension, optic disc edema, papilledema, Patton's Lines
-
 Mild Patton's Lines in IIH - Initial Photo
Mild Patton's Lines in IIH - Initial Photo
Jan 16 2019 by John S. King, MD
18-year-old African American female with increased BMI with a history of headaches, nausea, transient diplopia and vision loss that she notices when getting up from her bed (and goes away after standing upright) for the last two weeks. Went to PCP and was treated for the flu, and after no improvement and visual symptoms known, was sent to ED. MRI did not show any masses and showed empty sella turcia. Vision 20/30 OD and 20/20 OS; no RAPD; IOP 15OU; no anterior segment or vitreous inflammation; discs are elevated with obscuration of the disc margins and some of the smaller vessels; there are no SVPs; there are mild Patton's lines temporally (see Initial Photos). The optic disc cube shows 360 degrees of RNFL thickening (see OCT). Was referred to near-ophthalmologist, Dr. Doyle. She obtained additional work-up, and LP opening pressure was high, and MRV showed bilateral transverse sinus stenosis. Patient showed steady improvement with medical therapy, that included weight loss and oral diamox. On her last visit with Dr. Doyle, vision has remained stable at 20/20-20/25 without an enlarged blindspot; there are SVPs and optic disc edema has resolved (see Post Treatment Photos); she is currently on 1000 mg of diamox and has lost 15 pounds, and no stinting procedure needed.
Photographer: Gretchen Harper
Imaging device: Topcon 50
Condition/keywords: idiopathic intracranial hypertension, optic disc edema, papilledema, Patton's Lines
-
 Biopsy Proven Giant Cell Arteritis
Biopsy Proven Giant Cell Arteritis
Oct 15 2018 by Darin R. Goldman, MD
83-year-old male with biopsy-proven giant cell arteritis OU and old BRVO OS.
Photographer: Crystal Esparza, BS, COA, Retina Group of Florida
Imaging device: Topcon TRC 50DX
Condition/keywords: branch retinal vein occlusion (BRVO), giant cell arteritis, optic disc edema, papilledema
-
 Radiation Retinopathy resulting in Retinal Vascular Occlusive Disease
Radiation Retinopathy resulting in Retinal Vascular Occlusive Disease
Sep 11 2018 by Olivia Rainey
Ultra-wide field fluorescein angiography of a 57-year-old male s/p I-125 brachytherapy for malignant melanoma affecting his right eye. The patient’s radiation retinopathy has resulted in retinal vascular occlusive disease and optic nerve edema.
Photographer: Olivia Rainey
Imaging device: Optos
Condition/keywords: branch retinal vein occlusion (BRVO), fluorescein angiogram (FA), I-125 brachytherapy, malignant melanoma, optic disc edema, Optos, radiation retinopathy, ultra-wide field imaging
-
 OCT Through Foveal Area in Macular Infarction Secondary to Subconjunctival Gentamicin Injection
OCT Through Foveal Area in Macular Infarction Secondary to Subconjunctival Gentamicin Injection
May 16 2014 by Arwa Azmeh, MD, PhD
A 20-year-old male suffered from diplopia since age one. He was diagnosed to have acquired fourth nerve palsy in his left eye. VA at time of diagnosis was 20/20 in OU and fundus exam was WNL in OU. His history reaveled no other complaints. 3 days ago he underwent left superior oblique tucking for relief of his diplopia.The surgery was uneventful and at the end of surgery subconjunctival gentamicin was injected. Immediately following surgery his VA in OS decreased from 20/20 to complete loss of central vision and sensation of HM from the periphery. He was referred to us 3 days after surgery. At time of referral fundus exam of his left eye revealed macular infarction with cherry red spot appearance with few retinal hemorrhages , mild optic disc edema and CWS surrounding optic disc. Peripheral retina had normal color and appearance. The vitreous was clear. Anterior segment was quiet. IOP was WNL. Macular OCT was consistent with macular infarction. FA revealed delay in central retinal artery filling as fluorescein started to appear in the arteries at the level of the optic disc at 28 sec, and in the retinal veins at 38 sec. Macular area remained to be non-perfused throughout the whole FA. In late phases staining of blood vessels walls was noticed. The "wipe out" of large vessels and capillaries persisted in the central area. OCT through foveal area showed diffuse thickening of the retina with severe elevation in the fovea, reduced backscattering from the outer layers of the retina and enhanced reflectivity from the inner retina, due to ischemia. Complete blood count and cardiovascular study were WNL. The final diagnosis was macular infarction secondary to subconjunctival gentamicin injection.
Imaging device: OCT
Condition/keywords: macular infarction, subconjunctival gentamicin
-
 Late FA Phase of Macular Infarction Secondary to Subconjunctival Gentamicin Injection
Late FA Phase of Macular Infarction Secondary to Subconjunctival Gentamicin Injection
May 16 2014 by Arwa Azmeh, MD, PhD
A 20-year-old male suffered from diplopia since age one. He was diagnosed to have acquired fourth nerve palsy in his left eye. VA at time of diagnosis was 20/20 in OU and fundus exam was WNL in OU. His history revealed no other complaints. 3 days ago he underwent left superior oblique tucking for relief of his diplopia.The surgery was uneventful and at the end of surgery subconjunctival gentamicin was injected. Immediately following surgery his VA in OS decreased from 20/20 to complete loss of central vision and sensation of HM from the periphery. He was referred to us 3 days after surgery. At time of referral fundus exam of his left eye revealed macular infarction with cherry red spot appearance with few retinal hemorrhages, mild optic disc edema and CWS surrounding optic disc. Peripheral retina had normal color and appearance. The vitreous was clear. Anterior segment was quiet. IOP was WNL. Macular OCT was consistent with macular infarction. FA revealed delay in central retinal artery filling as fluorescein started to appear in the arteries at the level of the optic disc at 28 sec, and in the retinal veins at 38 sec. Macular area remained to be non-perfused throughout the whole FA. In late phases staining of blood vessels walls was noticed. The "wipe out" of large vessels and capillaries persisted in the central area. OCT through foveal area showed diffuse thickening of the retina with severe elevation in the fovea, reduced backscattering from the outer layers of the retina and enhanced reflectivity from the inner retina, due to ischemia. Complete blood count and cardiovascular study were WNL. The final diagnosis was macular infarction secondary to subconjunctival gentamycin injection.
Imaging device: OCT
Condition/keywords: macular infarction, subconjunctival gentamicin

 Loading…
Loading…