Search results (64 results)
-
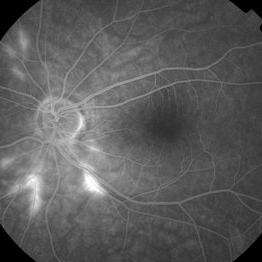
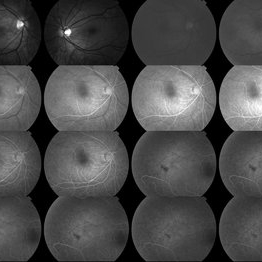
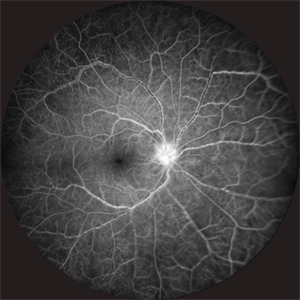 Takayasu Retinopathy
Takayasu Retinopathy
Apr 30 2025 by Vishal Agrawal, MD, FRCS,FACS,FASRS
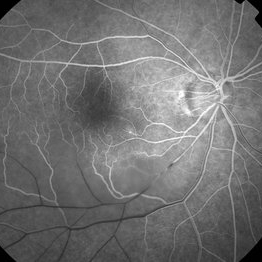
Fundus fluorescein angiography image of a young girl with diagnosed Takayasu arteritis who presented with complains of diminished vision in both eyes. FFA shows complete absence of venous filling with segmented blood column secondary to CRAO with peripheral avascular area.
Photographer: Dr Ayushi Gupta
Imaging device: Clarus 700
Condition/keywords: CRAO, Takayasus disease
-
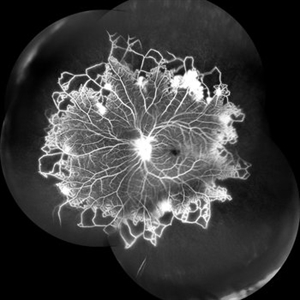
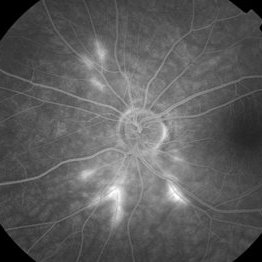
 Takayasu Retinopathy
Takayasu Retinopathy
Apr 30 2025 by Vishal Agrawal, MD, FRCS,FACS,FASRS
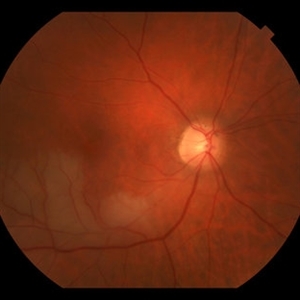
Fundus fluorescein angiography image of a young girl with diagnosed Takayasu arteritis who presented with complains of diminished vision in both eyes. FFA shows complete absence of venous filling with segmented blood column secondary to CRAO with peripheral avascular area.
Photographer: Dr Ayushi Gupta
Imaging device: Clarus 700
Condition/keywords: calcified drusen, CRAO, takayasu arteritis
-
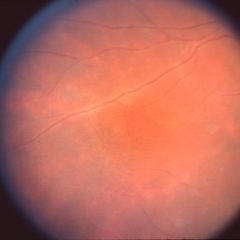
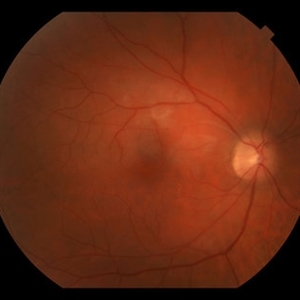
 Ocular Toxoplasmosis
Ocular Toxoplasmosis
Sep 24 2024 by Gustavo Uriel Fonseca Aguirre
24-year-old patient with a history of retinochoroiditis due to toxoplasmosis in the right eye, a focus of retinochoroiditis reactivation of toxoplasmosis is observed.
Photographer: Gustavo U. Fonseca Aguirre, Fundación Hospital Nuestra Señora de la Luz, Ciudad de México
Condition/keywords: Kyrieleis arteritis, toxoplasmosis reactivation
-
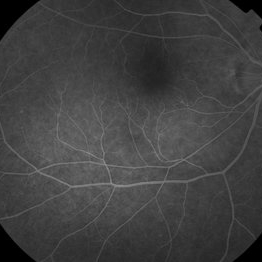
 Vascular Non Perfusion in Takayasu Arteritis
Vascular Non Perfusion in Takayasu Arteritis
Feb 6 2024 by SHILPI H NARNAWARE, ICO ( Retina) , FAICO ( Vitreo-Retina)
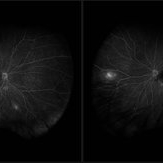
A case of 16 year-old female with combined RD in RE. Fundus examination & FFA revealed 360 degrees non-perfusion in periphery in non-symptomatic eye.
Photographer: Shilpi Narnaware, Sarakshi Netralaya , Nagpur, Maharashtra , India
Imaging device: Mirante ( by Nidek)
Condition/keywords: CNP areas, takayasu arteritis
-
Kyrieleis Plaques
Jan 12 2022 by Joshua S Agranat, MD
Prominent kyrieleis plaques in a patient with toxoplasmosis.
Condition/keywords: Kyrieleis arteritis, kyrieleis plaques, toxoplasmosis
-
 Combined GCA and AH
Combined GCA and AH
Oct 27 2020 by Nathan C. Steinle, MD
This patient demonstrates two rare diseases in one image: giant cell arteritis choroidal vascular ischemia with asteroid hyalosis. Delayed choroidal filling can be a presenting sign of giant cell arteritis, which is a life-threatening disease.
Photographer: Nancy Gutierrez
Imaging device: Optos
Condition/keywords: asteroid hyalosis, giant cell arteritis
-
 Combined GCA and AH
Combined GCA and AH
Oct 27 2020 by Nathan C. Steinle, MD
This patient demonstrates two rare diseases in one image: giant cell arteritis choroidal vascular ischemia with asteroid hyalosis. Delayed choroidal filling can be a presenting sign of giant cell arteritis, which is a life-threatening disease.
Photographer: Nancy Gutierrez
Imaging device: Optos
Condition/keywords: asteroid hyalosis, giant cell arteritis
-
 Segmental Periarteritis in Toxoplasmosis
Segmental Periarteritis in Toxoplasmosis
Apr 8 2019 by Gary R. Cook, MD, FACS
Fundus photograph of segmental periarteritis secondary to ocular toxoplasmosis in the right eye of a 19-year-old white male.
Condition/keywords: segmental periarteritis, toxoplasmosis
-
 Slide 11-26
Slide 11-26
Feb 26 2019 by Lancaster Course in Ophthalmology
Verhoeff-Van Gieson stain of same segment to show rupture of elastic intima ( x40). (Scheie Eye Institute, No. 3571.)
Condition/keywords: elastic intima, rupture, temporal arteritis
-
 Slide 11-25
Slide 11-25
Feb 26 2019 by Lancaster Course in Ophthalmology
Segment of temporal artery in a patient with temporal arteritis. Inflammatory infiltrate and thickening of all layers (x 101).
Condition/keywords: temporal arteritis
-
Slide 1-27
Feb 19 2019 by Lancaster Course in Ophthalmology
Acute arteritis in an orbital inflammatory pseudotumor. Arterial wall is edematous and thickened with PMNs, lymphocytes, and macrophages. Eosinophils are seen in the tissue at right. (H&E stain)
Condition/keywords: arteritis, edematous, eosinophils, polymorphonuclear leukocytes (PMNs), pseudotumor
-
 Biopsy Proven Giant Cell Arteritis
Biopsy Proven Giant Cell Arteritis
Oct 15 2018 by Darin R. Goldman, MD
83-year-old male with biopsy-proven giant cell arteritis OU and old BRVO OS.
Photographer: Crystal Esparza, BS, COA, Retina Group of Florida
Imaging device: Topcon TRC 50DX
Condition/keywords: branch retinal vein occlusion (BRVO), giant cell arteritis, optic disc edema, papilledema
-
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and superotemporal BRAO OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG (this FA is one month post recurrence with resolved inferotemporal BRAO after prednisone taper and increase in IMT). She is stable and doing well with 20/20 vision in both eyes.
Photographer: Kay Dalby
Imaging device: Topcon
Condition/keywords: retinal vasculitis, Susac's syndrome
-
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO superotemporally OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG (FA shows a inferotemporally BRAO while adjusting IMT). She is stable and doing well with 20/20 vision in both eyes.
Photographer: Stacey Coleman
Imaging device: Topcon
Condition/keywords: branch retinal artery occlusion (BRAO), retinal vasculitis, Susac's syndrome
-
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO superotemporally OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG (FA shows a inferotemporally BRAO while adjusting IMT). She is stable and doing well with 20/20 vision in both eyes.
Photographer: Stacey Coleman
Imaging device: Topcon
Condition/keywords: branch retinal artery occlusion (BRAO), retinal vasculitis, Susac's syndrome
-
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO OD without embolus, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG (photo of BRAO inferotemporally while adjusting immunosuppression). She is stable and doing well with 20/20 vision in both eyes.
Photographer: Stacey Coleman
Imaging device: Topcon
Condition/keywords: retinal vasculitis, Susac's syndrome
-
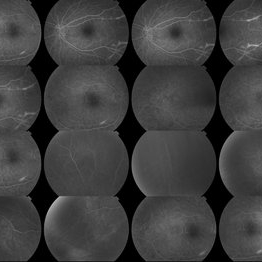
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG (FA shows a recurrence/worsening while adjusting IMT). She is stable and doing well with 20/20 vision in both eyes.
Photographer: Macey Highfill
Imaging device: Topcon
Condition/keywords: retinal vasculitis, Susac's syndrome
-
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG (FA shows a recurrence/worsening while adjusting IMT). She is stable and doing well with 20/20 vision in both eyes.
Photographer: Kay Dalby
Imaging device: Topcon
Condition/keywords: retinal vasculitis, Susac's syndrome
-
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG (FA shows a recurrence/worsening while adjusting IMT). She is stable and doing well with 20/20 vision in both eyes.
Photographer: Kay Dalby
Imaging device: Topcon
Condition/keywords: retinal vasculitis, Susac's syndrome
-
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG Background: 46yo WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG (FA shows a recurrence/worsening while adjusting IMT). She is stable and doing well with 20/20 vision in both eyes.
Photographer: Kay Dalby
Imaging device: Topcon
Condition/keywords: retinal vasculitis, Susac's syndrome
-
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG. She is stable and doing well with 20/20 vision in both eyes (most recent FA)
Photographer: Kay Dalby
Imaging device: Topcon
Condition/keywords: retinal vasculitis, Susac's syndrome
-
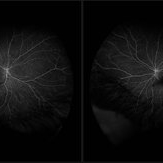
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
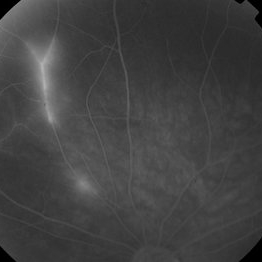
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and superotemporal BRAO OD, and bilateral arteritis (initial FAs). She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathioprine, and MTX, and has had the best reponse to IVIG. She is stable and doing well with 20/20 vision in both eyes.
Photographer: Maycey Highfill
Imaging device: Topcon
Condition/keywords: Susac's syndrome
-
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO superitemporally OD, and bilateral arteritis (see initial FA). She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathioprine, and MTX, and has had the best reponse to IVIG. She is stable and doing well with 20/20 vision in both eyes.
Photographer: Maycey Highfill
Imaging device: Topcon
Condition/keywords: Susac's syndrome
-
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO superotemporally OD (see photo), and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathioprine, and MTX, and has had the best reponse to IVIG. She is stable and doing well with 20/20 vision in both eyes.
Photographer: Macey Highfill
Imaging device: Topcon
Condition/keywords: Susac's syndrome
-
 Temporal Arteritis
Temporal Arteritis
Jan 7 2015 by H. Michael Lambert, MD
Chalky white swollen left optic nerve.
Condition/keywords: temporal arteritis

 Loading…
Loading…