Search results (157 results)
-
 Regressing Choroidal Melanoma
Regressing Choroidal Melanoma
Mar 10 2025 by Virginia Gebhart
56 year old male 4 months s/p plaque brachytherapy for choroidal melanoma. Tumor is regressing, there is an exudative detachment with worsening SRF. Treated with Avastin to promote hopeful improvement of the SRF
Photographer: Virginia Gebhart, Retina Consultants of Carolina
Imaging device: Optos California
Condition/keywords: brachytherapy, Choroidal melanoma, exudative detachment, melanoma
-
 Pre-Retinal Hemorrhage
Pre-Retinal Hemorrhage
Aug 22 2024 by Virginia Gebhart
51 year old female with moderate proliferative diabetic retinopathy, DME, as well as pre-retinal hemorrhage and likely NVE. Pt given Avastin in office and will return for PRP.
Photographer: Virginia Gebhart
Imaging device: Optos California
Condition/keywords: diabetic macular edema, macular edema, PDR with NVE (periphery), pre-retinal hemorrhage, proliferative diabetic retinopathy (PDR)
-
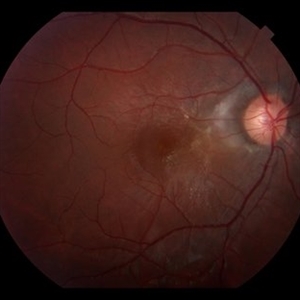
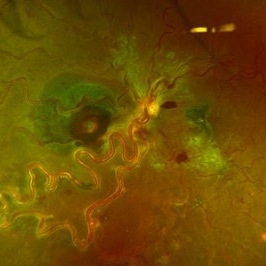 Left Eye Arteriovenous Malformation, Vein Occlusion and Ruptured Macroaneurysm
Left Eye Arteriovenous Malformation, Vein Occlusion and Ruptured Macroaneurysm
Feb 9 2024 by Sandra R Montezuma, MD
47 year old female presented with acute changes in vision in the left eye, flashes of light and a new supero temporal scotoma. No history of trauma. She has history of retina bleeding in 1998 when she was pregnant and had pre-eclampsia. She was told had a retina scar. Her VA was 20/500. Fundus exam revealed an arteriovenous malformation along inferonasal vessels with prominent tortuous vessels. The optic nerve was hyperemic and there was peripapillary pre-retinal hemorrhage. There is a central macula scar and retina hemorrhage in the macula and mid periphery. In the nasal mid periphery, there is a ruptured macroaneurysm with hemorrhage in all layers of the retina. There are diffuse IRH. Her OCT revealed abnormal foveal contour with intraretinal fluid, Outer retinal atrophy and increased hyperreflectivity of the inner retina layers. The patient was treated with avastin injections with some improvement of the vision and resolution of the intraretinal fluid. Her MRI was normal.
Photographer: University of Minnnesota
Condition/keywords: arteriovenous malformation, macroaneurysm, vein occlusion
-
 Central Retinal Vein Occlusion
Central Retinal Vein Occlusion
Apr 13 2023 by Virginia Gebhart
68-year-old male with Central Retinal Vein Occlusion with Macular Edema. Pt presented with VA of count fingers @ 5 ft. Pt was treated with Avastin
Photographer: Virginia Gebhart, Retina Consultants of Carolina
Imaging device: Topcon TRC 50DX
Condition/keywords: central retinal vein occlusion (CRVO)
-
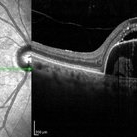 Pigment Epithelium Detachment, Secondary to AMD
Pigment Epithelium Detachment, Secondary to AMD
Mar 17 2023 by Ceara Donovan
Optical coherence tomography of a 76 year old woman with a Pigment Epithelium Detachment, Secondary to AMD affecting her right eye. Patient had no significant response to Avastin, Eylea, Lucentis 0.5, or Vabysmo and was switched to Beovu. Following Beovu intravitreal injection her edema improved on OCT. Patient's vision was sc20/200+1 at the time the image was taken.
Photographer: Ceara Donovan
Imaging device: Heidelberg Spectralis
Condition/keywords: exudative age-related macular degeneration, heidelberg spectralis, macular degeneration, optical coherence tomography (OCT), pigment epithelial detachment (PED), Sub-retinal fluid
-
 PPCNVM and Peripheral Drusen Seen on Optos FA
PPCNVM and Peripheral Drusen Seen on Optos FA
Apr 22 2020 by John S. King, MD
72-year-old white male c/o of distortion OS for about 2 months. 20/100 OS, normotensive, small grey-green subretinal area just temporal to the optic disc. FA shows leakage c/w a ppcnvm; there is some SR and IR leakage as well as staining of peripheral drusen and some window defects from cobblestone. Avastin was adminstered.
Photographer: Asli Ahmed
Imaging device: CA
Condition/keywords: drusen, peripapillary choroidal neovascularization (PPCNVM)
-
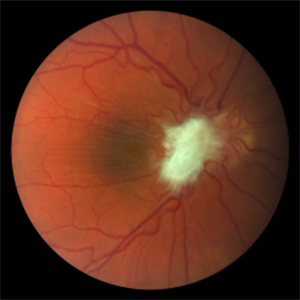
 Moyamoya: Photo OD of an Acute CRAO with CRA Sparing
Moyamoya: Photo OD of an Acute CRAO with CRA Sparing
Nov 17 2019 by John S. King, MD
60-year-old white female presented with five days of acute vision loss in the right eye. She was seen initially by referring doctor after hours five days ago and diagnosed with a CRAO and sent to ED to be evaluated stroke team. Right ICA was 100% closed but completely bypassed. She called four days later c/o redness and eye pain; at this point prominent iris vessels were seen, and she was sent to us. Her background history includes a diagnosis of moyamoya (underwent bilateral cerebral artery bypass 2015); atorvastatin for hypercholesterolemia; ASA; no hx of HTN or heart disease. She had a scleral buckle repair OD in 2017 and later developed a thick ERM, which was repaired in 2018; on her previous visit her acuity was noted at 20/40. On presentation her visual acuity was HM OD and 20/15 OS. IOP was 8 OD and 10 OS. There were prominent iris vessels in the right eye, no cell or flare, and an IOL. The posterior segment exam showed diffuse retinal whitening with attenuated vessels and boxcarring; there was sparing retinal whitening in a central area of the macula that appeared to be supplied by a cilio-retina artery. The FA showed very slow filling of the retinal vessels; there was some early perfusion secondary to the cilio-retinal artery. At 7 minutes there was still significant areas of non-perfusion, as well as macular ischemia. Avastin was administered, and one week later, PRP was performed. On the day PRP was performed, the irregular iris vessels had regressed completely. She said that she had a "sliver" of vision centrally in that eye; her acuity was CF 2' and IOP 12.
Photographer: Gretchen Harper
Imaging device: Topcon
Condition/keywords: central retinal artery occlusion (CRAO), cilioretinal sparing, moyamoya, neovascularization of iris (NVI)
-
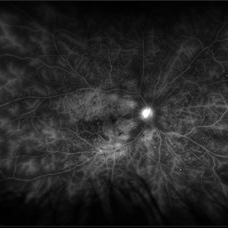
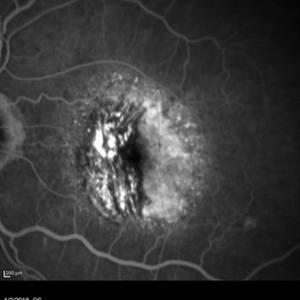
 Moyamoya: FA 52 Sec OD of an Acute CRAO with CRA Sparing
Moyamoya: FA 52 Sec OD of an Acute CRAO with CRA Sparing
Nov 17 2019 by John S. King, MD
60-year-old white female presented with five days of acute vision loss in the right eye. She was seen initially by referring doctor after hours five days ago and diagnosed with a CRAO and sent to ED to be evaluated stroke team. Right ICA was 100% closed but completely bypassed. She called four days later c/o redness and eye pain; at this point prominent iris vessels were seen, and she was sent to us. Her background history includes a diagnosis of moyamoya (underwent bilateral cerebral artery bypass 2015); atorvastatin for hypercholesterolemia; ASA; no hx of HTN or heart disease. She had a scleral buckle repair OD in 2017 and later developed a thick ERM, which was repaired in 2018; on her previous visit her acuity was noted at 20/40. On presentation her visual acuity was HM OD and 20/15 OS. IOP was 8 OD and 10 OS. There were prominent iris vessels in the right eye, no cell or flare, and an IOL. The posterior segment exam showed diffuse retinal whitening with attenuated vessels and boxcarring; there was sparing retinal whitening in a central area of the macula that appeared to be supplied by a cilio-retina artery. The FA showed very slow filling of the retinal vessels; there was some early perfusion secondary to the cilio-retinal artery. At 7 minutes there was still significant areas of non-perfusion, as well as macular ischemia. Avastin was administered, and one week later, PRP was performed. On the day PRP was performed, the irregular iris vessels had regressed completely. She said that she had a "sliver" of vision centrally in that eye; her acuity was CF 2' and IOP 12.
Photographer: Gretchen Harper
Imaging device: Topcon
Condition/keywords: central retinal artery occlusion (CRAO), cilioretinal sparing, moyamoya, neovascularization of iris (NVI)
-
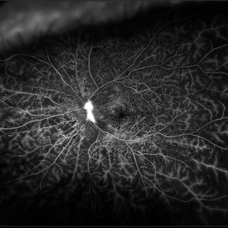
 Moyamoya: FA 2 Min OD of an Acute CRAO with CRA Sparing
Moyamoya: FA 2 Min OD of an Acute CRAO with CRA Sparing
Nov 17 2019 by John S. King, MD
60-year-old white female presented with five days of acute vision loss in the right eye. She was seen initially by referring doctor after hours five days ago and diagnosed with a CRAO and sent to ED to be evaluated stroke team. Right ICA was 100% closed but completely bypassed. She called four days later c/o redness and eye pain; at this point prominent iris vessels were seen, and she was sent to us. Her background history includes a diagnosis of moyamoya (underwent bilateral cerebral artery bypass 2015); atorvastatin for hypercholesterolemia; ASA; no hx of HTN or heart disease. She had a scleral buckle repair OD in 2017 and later developed a thick ERM, which was repaired in 2018; on her previous visit her acuity was noted at 20/40. On presentation her visual acuity was HM OD and 20/15 OS. IOP was 8 OD and 10 OS. There were prominent iris vessels in the right eye, no cell or flare, and an IOL. The posterior segment exam showed diffuse retinal whitening with attenuated vessels and boxcarring; there was sparing retinal whitening in a central area of the macula that appeared to be supplied by a cilio-retina artery. The FA showed very slow filling of the retinal vessels; there was some early perfusion secondary to the cilio-retinal artery. At 7 minutes there was still significant areas of non-perfusion, as well as macular ischemia. Avastin was administered, and one week later, PRP was performed. On the day PRP was performed, the irregular iris vessels had regressed completely. She said that she had a "sliver" of vision centrally in that eye; her acuity was CF 2' and IOP 12.
Photographer: Gretchen Harper
Imaging device: Topcon
Condition/keywords: central retinal artery occlusion (CRAO), cilioretinal sparing, moyamoya, neovascularization of iris (NVI)
-
 Moyamoya: FA 3:25 OD of an Acute CRAO with CRA Sparing
Moyamoya: FA 3:25 OD of an Acute CRAO with CRA Sparing
Nov 17 2019 by John S. King, MD
60-year-old white female presented with five days of acute vision loss in the right eye. She was seen initially by referring doctor after hours five days ago and diagnosed with a CRAO and sent to ED to be evaluated stroke team. Right ICA was 100% closed but completely bypassed. She called four days later c/o redness and eye pain; at this point prominent iris vessels were seen, and she was sent to us. Her background history includes a diagnosis of Moyamoya (underwent bilateral cerebral artery bypass 2015); atorvastatin for hypercholesterolemia; ASA; no hx of HTN or heart disease. She had a scleral buckle repair OD in 2017 and later developed a thick ERM, which was repaired in 2018; on her previous visit her acuity was noted at 20/40. On presentation her visual acuity was HM OD and 20/15 OS. IOP was 8 OD and 10 OS. There were prominent iris vessels in the right eye, no cell or flare, and an IOL. The posterior segment exam showed diffuse retinal whitening with attenuated vessels and boxcarring; there was sparing retinal whitening in a central area of the macula that appeared to be supplied by a cilio-retina artery. The FA showed very slow filling of the retinal vessels; there was some early perfusion secondary to the cilio-retinal artery. At 7 minutes there was still significant areas of non-perfusion, as well as macular ischemia. Avastin was administered, and one week later, PRP was performed. On the day PRP was performed, the irregular iris vessels had regressed completely. She said that she had a "sliver" of vision centrally in that eye; her acuity was CF 2' and IOP 12.
Photographer: Gretchen Harper
Imaging device: Topcon
Condition/keywords: central retinal artery occlusion (CRAO), cilioretinal sparing, moyamoya, neovascularization of iris (NVI)
-
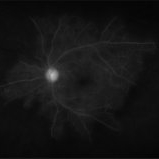
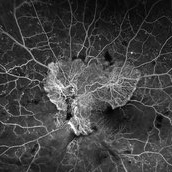
 Moyamoya: FA 7 Min OD of an Acute CRAO with CRA Sparing
Moyamoya: FA 7 Min OD of an Acute CRAO with CRA Sparing
Nov 17 2019 by John S. King, MD
60-year-old white female presented with five days of acute vision loss in the right eye. She was seen initially by referring doctor after hours five days ago and diagnosed with a CRAO and sent to ED to be evaluated stroke team. Right ICA was 100% closed but completely bypassed. She called four days later c/o redness and eye pain; at this point prominent iris vessels were seen, and she was sent to us. Her background history includes a diagnosis of Moyamoya (underwent bilateral cerebral artery bypass 2015); atorvastatin for hypercholesterolemia; ASA; no hx of HTN or Heart Disease. She had a scleral buckle repair OD in 2017 and later developed a thick ERM, which was repaired in 2018; on her previous visit her acuity was noted at 20/40. On presentation her visual acuity was HM OD and 20/15 OS. IOP was 8 OD and 10 OS. There were prominent iris vessels in the right eye, no cell or flare, and an IOL. The posterior segment exam showed diffuse retinal whitening with attenuated vessels and boxcarring; there was sparing retinal whitening in a central area of the macula that appeared to be supplied by a cilio-retina artery. The FA showed very slow filling of the retinal vessels; there was some early perfusion secondary to the cilio-retinal artery. At 7 minutes there was still significant areas of non-perfusion, as well as macular ischemia. Avastin was administered, and one week later, PRP was performed. On the day PRP was performed, the irregular iris vessels had regressed completely. She said that she had a "sliver" of vision centrally in that eye; her acuity was CF 2' and IOP 12.
Photographer: Gretchen Harper
Imaging device: Topcon
Condition/keywords: central retinal artery occlusion (CRAO), cilioretinal sparing, moyamoya, neovascularization of iris (NVI)
-
 Subretinal Fibrosis (PPCNVM and POHS) OS
Subretinal Fibrosis (PPCNVM and POHS) OS
Sep 18 2019 by John S. King, MD
57-year-old white male with history of PPCNVM OS and POHS OU here for a routine visit. History of avastin in 2014, and stable since then. Va OS 20/20. PP scar with macular subretinal fibrosis. No heme or exudates. CR spot supero-nasally.
Photographer: Shelly Blair
Imaging device: Topcon 50
Condition/keywords: choroidal neovascular membrane (CNVM), ocular histoplasmosis syndrome (OHS), peripapillary choroidal neovascularization (PPCNVM), presumed ocular histoplasmosis syndrome (POHS)
-
 Plaquenil Toxicity
Plaquenil Toxicity
Jun 20 2019 by Olivia Rainey
Ultra-wide field fundus autofluorescence photograph of a 60-year-old female with plaquenil toxicity affecting both eyes. Patient was taking plaquenil for management of Lupus, but discontinued use in 2011, but continues to be affected with severe progression of toxicity. Patient developed macular edema affecting her right eye and has received 5 Avastin injections.
Photographer: Olivia Rainey
Imaging device: Optos
Condition/keywords: autofluorescence imaging, focal pigmentary changes, fundus autofluorescence (FAF), macular edema, Optos, plaquenil toxicity, ultra-wide field imaging
-
 Proliferative Diabetic Retinopathy with Retinal Ischemia
Proliferative Diabetic Retinopathy with Retinal Ischemia
Mar 29 2019 by Olivia Rainey
Ultra-wide field fluorescrein angiogram of a 42-year-old female with proliferative diabetic retinopathy with retinal ischemia affecting her right eye. Patient had been noticing a vision decline and floaters over the past few months. She was treated with Avastin in her right eye and then her left one week later.
Photographer: Olivia Rainey
Imaging device: Optos
Condition/keywords: diabetes, diabetic macular edema, fluorescein angiogram (FA), fluorescein leakage, late phase, neovascularization of the disc (NVD), Optos, proliferative diabetic retinopathy (PDR), retinal ischemia, ultra-wide field imaging
-
 Proliferative Diabetic Retinopathy with Retinal Ischemia
Proliferative Diabetic Retinopathy with Retinal Ischemia
Mar 29 2019 by Olivia Rainey
Ultra-wide field fluorescrein angiogram of a 42-year-old female with proliferative diabetic retinopathy with retinal ischemia affecting her left. Patient had been noticing a vision decline and floaters over the past few months. She was treated with Avastin in her right eye and then her left one week later.
Photographer: Olivia Rainey
Imaging device: Optos
Condition/keywords: diabetes, diabetic macular edema, early phase, fluorescein angiogram (FA), fluorescein leakage, neovascularization of the disc (NVD), Optos, proliferative diabetic retinopathy (PDR), retinal ischemia, ultra-wide field imaging
-
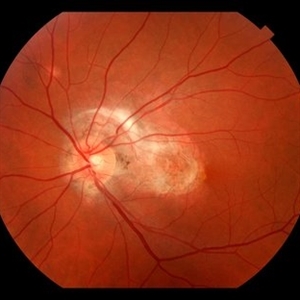
 Silicon Droplet in the Cup of Optic Nerve After Multiple Intravitreal Avastin Treatments
Silicon Droplet in the Cup of Optic Nerve After Multiple Intravitreal Avastin Treatments
Nov 1 2018 by Tammy Mclaughlin
Fundus photograph of a 68-year-old man with silicon droplet in the cup of optic nerve after multiple intravitreal Avastin treatments.
Photographer: Tammy Mclaughlin, Carolina Retina Center, Sumter SC
Imaging device: Zeiss Visucam
Condition/keywords: optic nerve
-
 Pre-Retinal Fibrosis Following Endogenous Fungal Endophthalmitis
Pre-Retinal Fibrosis Following Endogenous Fungal Endophthalmitis
Aug 23 2018 by Matthew Dombrow, MD
20-year-old male presents with posterior uveitis with a chain of white infiltrates stemming from the optic nerve. While treated, his infiltrates retracted and hemorrhage occured. Neovascularization of the disc developed and underwent Avastin treatment in addition to his oral anti-fungals and intravitreal anti-fungals. Patient was lost to follow up and presented with severe pre-retinal fibrosis 6 years later. Acuity is 20/40-1 with significant metamorphopsia.
Photographer: Patricia Candrea, COA, Connecticut Retina Consultants, LLC
Imaging device: Canon
Condition/keywords: pre-retinal membrane
-
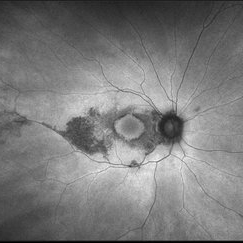
 Proliferative Diabetic Retinopathy with Neovascular Glaucoma
Proliferative Diabetic Retinopathy with Neovascular Glaucoma
Jul 12 2018 by Nichole Lewis
68-year-old male with proliferative diabetic retinopathy, severe capillary nonperfusion and neovascular glaucoma. Treated with Avastin intra-ocular injection and future pan-retinal photocoagulation. VA 20/300.
Photographer: Nichole Lewis
Condition/keywords: capillary nonperfusion, diabetes, neovascular glaucoma, non-perfusion, proliferative diabetic retinopathy (PDR)
-
 ROP FA OS
ROP FA OS
Apr 27 2018 by Brenda Fallas
4-month-old baby with regressed ROP post-Avastin.
Photographer: Brenda Fallas, Bascom Palmer Eye Institute, Miami, FL
Imaging device: RETCAM III 130 degree lens montage
Condition/keywords: FA late phase leakage, fluorescein angiogram (FA), retinopathy of prematurity (ROP)
-
 ROP FA OD
ROP FA OD
Apr 27 2018 by Brenda Fallas
4-month-old baby with regressed ROP post-Avastin.
Photographer: Brenda Fallas, Bascom Palmer Eye Institute, Miami, FL
Imaging device: RETCAM III 130 degree lens mongtage
Condition/keywords: FA late phase leakage, fluorescein angiogram (FA), retina, retinopathy of prematurity (ROP)
-
 POHS-CNVM
POHS-CNVM
Jan 7 2018 by John S. King, MD
17-year-old hx scotoma a year ago; 1-2 months of worsening scotoma; small chorio-retinal punched out lesions in mid-periph; midperipheral curvilinear pigment band in inf 180 degrees; staining and leakage on FA; avastin administered.
Imaging device: Topcon
Condition/keywords: choroidal neovascular membrane (CNVM), presumed ocular histoplasmosis syndrome (POHS)
-
 Neovascular AMD with Active CNV
Neovascular AMD with Active CNV
Jan 2 2018 by Carolyn Daley
30 degree fluorescein angiogram of an 80-year-old woman with neovascular AMD with active CNV in the left eye. Patient is being treated with Avastin.
Photographer: Carolyn Daley, Retina Specialists of Michigan
Imaging device: Heidelberg Spectralis
Condition/keywords: 30 degrees, choroidal neovascularization (CNV), Heidelburg Spectralis, left eye, neovascular age-related macular degeneration (AMD)
-
 PDR with NVD and CRVO history
PDR with NVD and CRVO history
Dec 6 2017 by John S. King, MD
One year earlier she had a CRVO with lots of CME, treated once with avastin, and scheduled to be seen and treated a month later; at that time no nv and some cap dropout seen in FAZ area, but extent of dropout limited by heme, diffuse cme, and no wide field image at that time; lost to follow up until a year later; see above
Imaging device: Optos
Condition/keywords: central retinal vein occlusion (CRVO), diabetic retinopathy
-
Wet AMD treated with Avastin
Sep 19 2017 by Theodore Leng, MD, MS, FASRS
Wet AMD treated with Avastin.
Condition/keywords: Avastin, wet age-related macular degeneration (wet AMD)
-
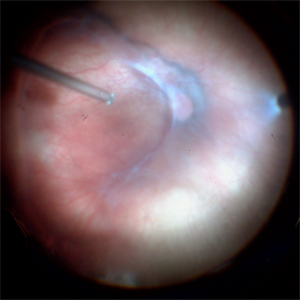 Stage 4a ROP
Stage 4a ROP
Apr 17 2017 by Alexandre Grandinetti, MD, PhD
Stage 4a retinopathy of prematurity in a 6-month-old baby previously treated with laser and intravitreal Avastin.
Photographer: Alexandre Grandinetti
Condition/keywords: retinopathy of prematurity (ROP), vitrectomy

 Loading…
Loading…