Search results (75 results)
-
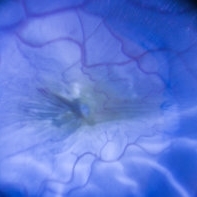 Per Operative Photo Post ILM Removal
Per Operative Photo Post ILM Removal
May 25 2017 by Manish Nagpal, MD, FRCS (UK), FASRS
Per operative photo immediately following ILM removal.
Photographer: manish nagpal
Imaging device: SONY HD SURGICAL MICROSCOPE CAMERA
Condition/keywords: dye, epiretinal membrane (ERM), internal limiting membrane (ILM) peeling, staining
-
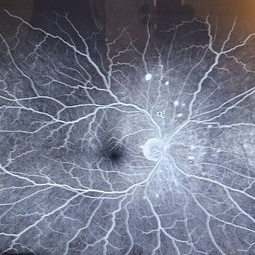
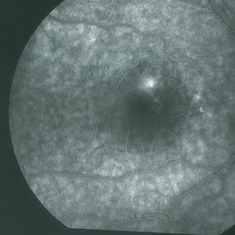
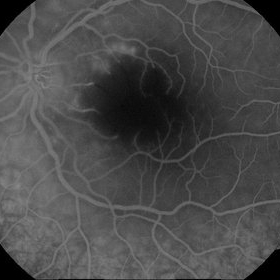
 Central Retinal Vein Occlusion: Case 1
Central Retinal Vein Occlusion: Case 1
Oct 12 2012 by Gregg T. Kokame, MD, MMM, FASRS
Dye-Transit FA
Photographer: Jaclyn Pisano, Retina Consultants of Hawaii
Imaging device: Topcon 50IA / Eschalon
Condition/keywords: central retinal vein occlusion (CRVO)
-
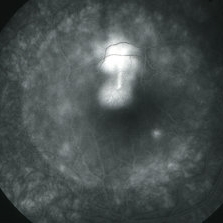
 Central Retinal Vein Occlusion: Case 1
Central Retinal Vein Occlusion: Case 1
Oct 12 2012 by Gregg T. Kokame, MD, MMM, FASRS
Dye-Transit FA
Photographer: Jaclyn Pisano, Retina Consultants of Hawaii
Imaging device: Topcon 50IA / Eschalon
Condition/keywords: central retinal vein occlusion (CRVO)
-
 Central Retinal Vein Occlusion: Case 1
Central Retinal Vein Occlusion: Case 1
Oct 12 2012 by Gregg T. Kokame, MD, MMM, FASRS
Dye-Transit FA
Photographer: Jaclyn Pisano, Retina Consultants of Hawaii
Imaging device: Topcon 50IA / Eschalon
Condition/keywords: central retinal vein occlusion (CRVO)
-
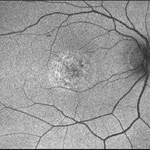
 Dye image
Dye image
Apr 13 2024 by Monica King
Unknown diagnosis. 35yr old female. Blind spots started to form.
Photographer: Dr. Becker, Colorado Eye Institute
Condition/keywords: Unknown diagnosis
-
 01 Unilateral Acute Idiopathic Maculopathy (UAIM) Pseudocolor Photograph OD
01 Unilateral Acute Idiopathic Maculopathy (UAIM) Pseudocolor Photograph OD
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of pt's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, patient mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT , diagnosed with CSCR and referred for retina evaluation. - ROS/ PMHx: negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - pseudocolor and FAF photos: RPE changes/ clumps with GA and stippled autofluorescense OD, unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, subfoveal ellipsoid zone atrophy with intact ELM with no CME or SRF OD, unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG and VF - patient rescheduled
Imaging device: Optos - California
Condition/keywords: unilateral acute idiopathic maculopathy
-
 02 Unilateral Acute Idiopathic Maculopathy (UAIM) - Pseudocolor Photograph OS
02 Unilateral Acute Idiopathic Maculopathy (UAIM) - Pseudocolor Photograph OS
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of pt's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, pt mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT , diagnosed with CSCR and referred for retina evaluation. - ROS/ PMHx: Negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - Pseudocolor and FAF photos: RPE changes/ clumps w/ GA and stippled autofluorescense OD, unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, Subfoveal ellipsoid zone atrophy w/ intact ELM W/No CME or SRF OD, Unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG & VF - patient rescheduled
Imaging device: Optos - California
Condition/keywords: unilateral acute idiopathic maculopathy
-
 03- Unilateral Acute Idiopathic Maculopathy (UAIM) - FAF OD
03- Unilateral Acute Idiopathic Maculopathy (UAIM) - FAF OD
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of patient's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, pt mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT , diagnosed w/ CSCR and referred for retina evaluation. - ROS/ PMHx: Negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - Pseudocolor & FAF photos: RPE changes/ clumps with GA and stippled autofluorescense OD, Unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, subfoveal ellipsoid zone atrophy with intact ELM with no CME or SRF OD, unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG & VF - pt rescheduled!
Imaging device: Optos - California
Condition/keywords: unilateral acute idiopathic maculopathy
-
 04- Unilateral Acute Idiopathic Maculopathy (UAIM) - FAF OS
04- Unilateral Acute Idiopathic Maculopathy (UAIM) - FAF OS
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of pateint's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, patient mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT, diagnosed with CSCR and referred for retina evaluation. - ROS/ PMHx: negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - pseudocolor and FAF photos: RPE changes/ clumps with GA & stippled autofluorescence OD, unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, subfoveal ellipsoid zone atrophy with intact ELM with no CME or SRF OD, unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG & VF - patient rescheduled
Imaging device: Optos - California
Condition/keywords: unilateral acute idiopathic maculopathy
-
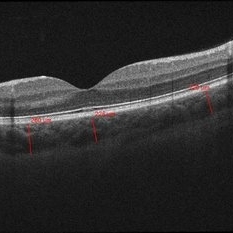
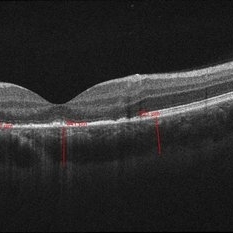 05- Unilateral Acute Idiopathic Maculopathy (UAIM) - OCT OD
05- Unilateral Acute Idiopathic Maculopathy (UAIM) - OCT OD
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of pt's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, pt mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT , diagnosed with CSCR and referred for retina evaluation. - ROS/ PMHx: Negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - Pseudocolor and FAF photos: RPE changes/ clumps w/ GA and stippled autofluorescense OD, unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, Subfoveal ellipsoid zone atrophy w/ intact ELM W/No CME or SRF OD, Unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG & VF - patient rescheduled
Imaging device: Zeiss-Cirrus 4000
Condition/keywords: unilateral acute idiopathic maculopathy
-
 05- Unilateral Acute Idiopathic Maculopathy (UAIM) - OCT OD2
05- Unilateral Acute Idiopathic Maculopathy (UAIM) - OCT OD2
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of pt's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, pt mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT , diagnosed with CSCR and referred for retina evaluation. - ROS/ PMHx: Negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - Pseudocolor and FAF photos: RPE changes/ clumps w/ GA and stippled autofluorescense OD, unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, Subfoveal ellipsoid zone atrophy w/ intact ELM W/No CME or SRF OD, Unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG & VF - patient rescheduled
Imaging device: Zeiss-Cirrus 4000
Condition/keywords: unilateral acute idiopathic maculopathy
-
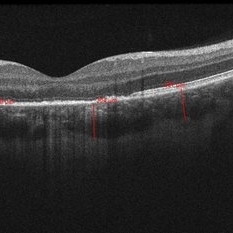
 06- Unilateral Acute Idiopathic Maculopathy (UAIM) - OCT OS
06- Unilateral Acute Idiopathic Maculopathy (UAIM) - OCT OS
Jul 24 2018 by Hosam Attia, MD
20-year-old white, male presented for initial evaluation with one week history of acute, sudden, painless loss of central vision in his right eye a week prior to presentation. - H/O short course of exogenous testosterone, Tamoxifen and Clomiphene intake ~ 2-3 weeks cycle, which was already stopped, prior to development of pt's symptoms. - H/O acute illness with generalized fatigue, malaise, URTI like symptoms and rash over the hands and chest, just prior to symptoms development, and upon further discussion, pt mentioned that few of his friends got sick around the same time. - Patient was seen the week prior by general ophthalmologist and was found to have SRF on OCT , diagnosed with CSCR and referred for retina evaluation. - ROS/ PMHx: Negative, healthy aside from the short illness described above - Denied any prior vision problems, similar episodes, trauma etc - VA Dsc OD: 20/400 OS:20/20 - anterior segment exam - unremarkable - posterior segment - macular RPE changes/ clumping with GA with no CME/ SRF or crystals OD, and unremarkable OS. - Pseudocolor and FAF photos: RPE changes/ clumps w/ GA and stippled autofluorescense OD, unremarkable OS. - HD SD-OCT: thickened choroid, thickened/ hypertrophied subfoveal RPE with hyper-reflective material on the apical side of the retinal pigment epithelium/apical debris, Subfoveal ellipsoid zone atrophy w/ intact ELM W/No CME or SRF OD, Unremarkable OS. - FA: Dye not available - ICG: deferred - mf-ERG & VF - patient rescheduled
Imaging device: Zeiss-Cirrus 4000
Condition/keywords: unilateral acute idiopathic maculopathy
-
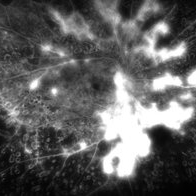 Active neovascularization in Proliferative Diabetic Retinopathy
Active neovascularization in Proliferative Diabetic Retinopathy
Jan 10 2018 by Peter H. Tang, MD, PhD
Fluorescein angiography image from a 46-year-old woman with uncontrolled proliferative diabetic retinopathy shows extensive dye leakage from active neovascularization.
Imaging device: Optos California
Condition/keywords: diabetes, diabetic retinopathy, fluorescein leakage, neovascularization elsewhere (NVE), neovascularization of the disc (NVD), pan-retinal photocoagulation (PRP), proliferative diabetic retinopathy (PDR)
-
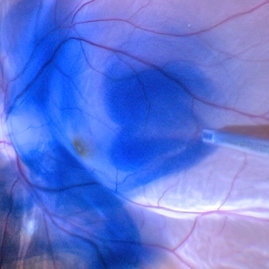
 BBG Dye injection to Stain ILM during Vitrectomy Surgery | Intra-Operative Still
BBG Dye injection to Stain ILM during Vitrectomy Surgery | Intra-Operative Still
Apr 28 2023 by Veer Singh, MS, FVRS, FMRF, FICO (Retina)
BBG Dye injection to Stain ILM during Vitrectomy Surgery | Intra-Operative Still
Photographer: Dr. Veer Singh
Condition/keywords: brilliant blue staining, ERM, ILM staining
-
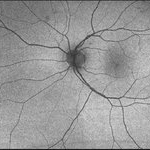
 Bilateral Central Serous Retinopathy
Bilateral Central Serous Retinopathy
Mar 26 2019 by Gary R. Cook, MD, FACS
Late-phase fluorescein angiogram image of the right eye of a 37-year-old white male showing pinpoint leak with late diffusion of dye from it superiorly and RPE irregularities nasal to fovea in a case of bilateral central serous retinopathy; VA = 20/20-2.
Imaging device: Topcon VT-50
Condition/keywords: central serous retinopathy (CSR), FA late phase, fluorescein angiogram (FA)
-
 Bilateral Central Serous Retinopathy
Bilateral Central Serous Retinopathy
Mar 26 2019 by Gary R. Cook, MD, FACS
Late-phase frame of FA of 37-year-old white male with acute CSR OD showing pooling of dye beneath the small central RPED centrally, a smokestack-type leak from the RPE defect just above it, and mild late pooling of dye outlining the large neurosensory macular detachment; VA = 20/80-1.
Imaging device: Topcon VT-50
Condition/keywords: central serous retinopathy (CSR), FA late phase, FA late phase leakage, neurosensory detachment of retina
-
Branch Retinal Artery Occlusion
Jun 24 2018 by Narciso F. Atienza, MD, MBA, FASRS, FPCS, FPAO.
62-year-old male patient with sudden loss of vision on the left eye for 3 days. Early arterial phase at 41 seconds after injection of the dye.
Photographer: Narciso Atienza, Jr. MD MBA, Legazpi Eye Center, Cardinal Santos Medical Center
Condition/keywords: branch retinal artery occlusion (BRAO)
-
 Brilliant Blue Dye Injected in a Case of Macular Hole to Stain the ILM
Brilliant Blue Dye Injected in a Case of Macular Hole to Stain the ILM
Feb 4 2022 by Manish Nagpal, MD, FRCS (UK), FASRS
Intraoperative still of a brilliant blue dye being injected to stain the ILM.
Photographer: Manish Nagpal, Director, Retina Foundation, Ahmedabad
Imaging device: Sony PMW -10 MD surgical camera
Condition/keywords: brilliant blue, ILM flap, ILM staining, macular hole, retina, retina surgery
-
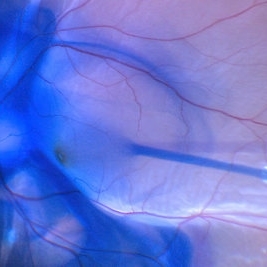
 Brilliant blue dye injection to stain ILM in a macular hole with retinal detachment
Brilliant blue dye injection to stain ILM in a macular hole with retinal detachment
Feb 4 2022 by Manish Nagpal, MD, FRCS (UK), FASRS
Intraoperative still of brilliant blue dye injection in process to initiate ILM peel in a patient who has a retinal detachment with a macular hole
Photographer: Manish Nagpal, Director, Retina Foundation, Ahmedabad
Imaging device: Sony PMW -10 MD surgical camera
Condition/keywords: brilliant blue, ILM flap, macular hole
-
 Brilliant Blue Dye Injection to Stain ILM in a Macular Hole with Retinal Detachment
Brilliant Blue Dye Injection to Stain ILM in a Macular Hole with Retinal Detachment
Feb 4 2022 by Manish Nagpal, MD, FRCS (UK), FASRS
Intraoperative still of a Brilliant blue dye injection being done to stain the ILM.
Photographer: Manish Nagpal, Director, Retina Foundation, Ahmedabad
Imaging device: Sony PMW -10 MD surgical camera
Condition/keywords: full thickness macular hole, macula, retina
-
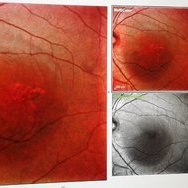
---thumb.jpg/image-square;max$300,300.ImageHandler) Brown/Mendis BJO 57:344, 1973
Brown/Mendis BJO 57:344, 1973
Feb 14 2013 by From the Collections of Thomas M. Aaberg, MD and Thomas M. Aaberg Jr., MD
reprints of figures 1 and 2 from the publication Brown and Mendis. Retinal arteritis complicating herpes zoster ophthalmicus. Br J Ophthalmol 1973;57:344-6. The left panel is a "fundus painting showing extensive exudate in areas of supply of narrowed and sheathed upper nasal and upper temporal retinal arterioles." The right panel is a fluorescein angiograph of the fundus, "demonstrating leakage of dye in area of exudation."
Condition/keywords: Herpes zoster, retinal arteriolar occlusion, retinal necrosis
-
Capillary Non-Perfusion
Aug 26 2019 by Narciso F. Atienza, MD, MBA, FASRS, FPCS, FPAO.
FA at 51 sec showing capillary non-perfusion and blocked fluoresence of the inferior macula and infero-temporal area with transit of dye on previously noted infero-temporal branch vein.
Photographer: Narciso F Atienza, Jr. MD, MBA
Imaging device: Topcon TRC
Condition/keywords: capillary nonperfusion
-
---thumb.jpg/image-square;max$300,300.ImageHandler) Central Retinal Artery Occlusion – Macular Branch
Central Retinal Artery Occlusion – Macular Branch
Mar 25 2013 by Ratimir Lazic, MD, PhD
FAG image of a 19 –year-old female. In late venous phase extended foveal avascular zone due to non perfusion with staining of dye proximal of occluded branches.
Photographer: Marko Lukic, MD
Imaging device: Zeis Visucam Lite 2
Condition/keywords: central retinal artery occlusion (CRAO)
-
 Central Retinal Artery Occlusion – Macular Branch
Central Retinal Artery Occlusion – Macular Branch
Mar 25 2013 by Ratimir Lazic, MD, PhD
FAG image of a 19 –year-old female. In late venous phase extended foveal avascular zone due to non perfusion with staining of dye proximal of occluded branches.
Photographer: Marko Lukic, MD
Imaging device: Zeis Visucam Lite 2
Condition/keywords: central retinal artery occlusion (CRAO)
-
 Central serous chorioretinopathy
Central serous chorioretinopathy
Apr 30 2015 by Mariam A Al-Feky, MD
A case of CSR phtographed on the Heidelberg fundus camera with multicolor image, infrared, blue reflectance and green reflectence predye injection, postdye injection and during dye injection and last image for the OCT. Fundus examination after dye injection showed a green spot nasal that was not detected predye injection. Multicolor image was retaken and that green spot is well evident in the multicolor image, the infrared relectance, blue and green reflectance. That green spot is corresponding to the leaky point in FFA and to a PED in OCT.
Photographer: Mariam AL-Feky
Condition/keywords: central serous retinopathy (CSR), leakage

 Loading…
Loading…