Search results (72 results)
-
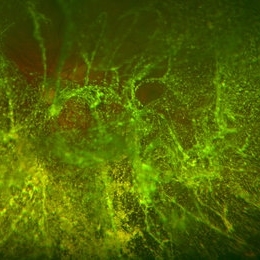 Extreme Asteroid Hyalosis
Extreme Asteroid Hyalosis
Apr 27 2016 by Matt Poe, COA
This patient was sent for a possible retinal detachment. Extreme difficult view of posterior pole due to asteroid hyalosis. After B-Scan was performed it was determined patient did not have a retinal detachment, only posterior vitreous detachment.
Photographer: Matt Poe, COA. Northwest Arkansas Retina Associates, Springdale, AR.
Condition/keywords: asteroid hyalosis, posterior vitreous detachment
-
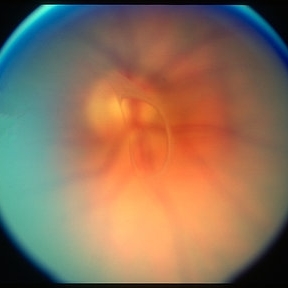
 Prominent Long Ciliary Nerve
Prominent Long Ciliary Nerve
Jan 25 2022 by Kachelle Brown
Ultra-wide field photograph of a 48-year-old female with a prominent long ciliary nerve. Patient presented asymptomatic, and was referred for a macula on retinal detachment. Patient was diagnosed with high myopia and a posterior vitreous detachment, and the physician discussed increased risk of floaters, myopic degeneration and retinal detachment associated with high myopia. -24.00 prior to cataract surgery OU per patient.
Photographer: Kachelle Brown
Imaging device: Optos California
Condition/keywords: fundus photograph, high myopia, long ciliary nerve, optos, right eye, ultra-widefield image
-
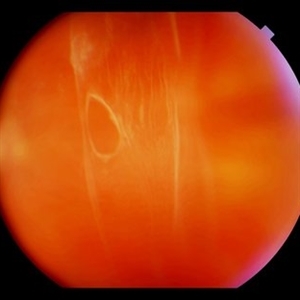
 Sudden Posterior Vitreous Detachment
Sudden Posterior Vitreous Detachment
Nov 9 2012 by Norman Byer
This 60-year-old man suffered a sudden posterior vitreous detachment which produced a large tractional retinal tear at 11:30 o’clock in this eye. This white cystic retinal tuft located at 9:30 also suffered minor injury at the same time as revealed in the next slide pair.
Condition/keywords: posterior vitreous detachment, white retinal tuft
-
 Posterior Vitreous Detachment
Posterior Vitreous Detachment
Sep 1 2020 by J. Sebag, MD, FACS, FRCOphth, FARVO
Left: Preset lens biomicroscopy of PVD in the left eye of a subject with a widely dilated pupil. The detached posterior vitreous cortex is seen (arrows) as is the optic disc and retinal vasculature (upper left). (courtesy of C. L. Trempe MD, Harvard Medical School, Boston, MA) [Sebag J: Vitreous – in Health & Disease Springer, New York, 2014; image © Springer Nature, reprinted with permission] Right: B-scan ultrasonography of PVD images the detached posterior vitreous cortex with a visible Weiss Ring.
Condition/keywords: posterior vitreous detachment
-
 Vitreous Hemorrhage
Vitreous Hemorrhage
Jul 10 2018 by Karen Panzegrau
SD-OCT of a 35-year-old female presenting with a vitreous hemorrhage of her left eye. Patient has active proliferative diabetic retinopathy, as well as a completed posterior vitreous detachment in the left eye.
Photographer: Karen Panzegrau
Condition/keywords: diabetes, Heidelburg Spectralis, left eye, optical coherence tomography (OCT), posterior vitreous detachment, proliferative diabetic retinopathy (PDR), vitreous hemorrhage
-
 Cystic Retinal Tuft
Cystic Retinal Tuft
Nov 9 2012 by Norman Byer
This is the same lesion as in the previous slide pair but the photograph was taken nine years later when the patient was 58-years-old soon after an acute posterior vitreous detachment. This demonstrates that posterior vitreous detachment can produce large retinal tears at these sites. However, it is important to emphasize that prophylactic treatment of cystic retinal tufts in the absence of a retinal tear would be very ill-advised because several hundred innocence and harmless lesions would have to be treated in order to prevent one tear of the retina.
Condition/keywords: cystic retinal tuft, posterior vitreous detachment, retinal tear
-
 Posterior vitreous detachment
Posterior vitreous detachment
Jan 11 2013 by Alex P. Hunyor, MD
Posterior vitreous detachment with prominent Weiss ring.
Condition/keywords: posterior vitreous detachment
-
 Weiss Ring
Weiss Ring
Jan 9 2019 by John S. King, MD
77-year-old white male with ERM and PVD OD; sheet of vitreous with weiss ring in the nasal mid-vitreous cavity.
Photographer: Macey Highfill, RN
Imaging device: Topcon 50
Condition/keywords: posterior vitreous detachment, Weiss ring
-
 ERM that Spontaneously Peeled
ERM that Spontaneously Peeled
Oct 8 2012 by David R. Chow, MD, FRCS(C)
An ERM that through follow-up sponateously separated with the development of PVD.
Condition/keywords: epiretinal membrane (ERM), posterior vitreous detachment
-
 Inactive Toxoplasmosis
Inactive Toxoplasmosis
Nov 9 2012 by Norman Byer
This 28-year-old man had inactive toxoplasmosis and presented with acute symptoms caused by this tractional retinal tear adjacent to a retinochorodial scar. He also had an acute posterior vitreous detachment which had torn this retinal operculum completely free. The next slide shows the same lesion. Note the early rolled edge on the left side of the tear.
Condition/keywords: acute posterior vitreous detachment, inactive toxoplasmosis, operculum, rolled edges of retina, tractional retinal tear
-
 Scleral Indentation
Scleral Indentation
Nov 9 2012 by Norman Byer
This is the same lesion with scleral indentation. You can see the small discrete preretinal hemorrhage and the sharply circumscribed area of elevated retina with subretinal fluid beneath it. No retinal break is visible, but the posterior vitreous is detached and exerting traction at this site. The area was surrounded with argon laser treatment the same day as the initial examination.
Condition/keywords: posterior vitreous detachment, preretinal hemorrhage, scleral indentation, subretinal fluid, vitreous traction
-
 Acute Posterior Vitreous Detachment
Acute Posterior Vitreous Detachment
Nov 9 2012 by Norman Byer
This large and complicated retinal tear in a 51-year-old man resulted from an acute posterior vitreous detachment which concentrated its tractional forces around this area of lattice degeneration. Because of the powerful traction, there is an additional central tear splitting the large retinal flap and almost severing one of its arms. The traction was strong enough to completely rupture the blood vessel just to the left of the flap. Marking the ruptured peripheral end of the blood vessel is a yellow depigmented thrombus.
Condition/keywords: acute posterior vitreous detachment, depigmented thrombus, lattice degeneration, retinal tear, tractional retinal detachment
-
 Acute Retinal Detachment
Acute Retinal Detachment
Nov 9 2012 by Norman Byer
This 54-year-old man was referred because of sudden symptoms in his opposite eye in which he had suffered an acute retinal detachment secondary to a horseshoe tear around lattice degeneration. During the examination, the fellow eye shown here was also found to have this large horseshoe tear about 1 o’clock hour (4 disc diameters) in size. A tear occurred around a lattice lesion which is present on the flap but is out of focus. This tear had been asymptomatic even though it was caused by a posterior vitreous detachment and illustrates that even very large tears may produce no symptoms or mild symptoms that are easily overlooked.
Condition/keywords: lattice degeneration, posterior vitreous detachment
-
 Astrocytic Hamartoma
Astrocytic Hamartoma
Feb 27 2025 by Daniel Davis, OCT-C
Color fundus photo of 55-year-old female with Astrocytic Hamartoma in association with tuberous sclerosis. No treatment options available, benign. Other findings include; Posterior Vitreous Detachment, Vitreous Hemorrhage, Hereditary Retinal Dystrophy, Vitreous Opacities, Hypertensive Retinopathy.
Photographer: Daniel Davis, OCT-C
Imaging device: Optos California
Condition/keywords: color fundus photograph
-
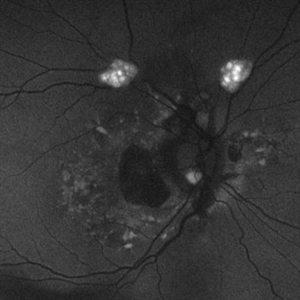 Astrocytic Hamartoma
Astrocytic Hamartoma
Feb 27 2025 by Daniel Davis, OCT-C
Fundus autofluorescence photo of 55-year-old female with astrocytic hamartoma in association with tuberous sclerosis. No treatment options available, benign. Other findings include; Posterior Vitreous Detachment, Vitreous Hemorrhage, Hereditary Retinal Dystrophy, Vitreous Opacities, Hypertensive Retinopathy.
Photographer: Daniel Davis, OCT-C
Imaging device: Optos California
Condition/keywords: astrocytic hamartoma, fundus autofluorescence (FAF)
-
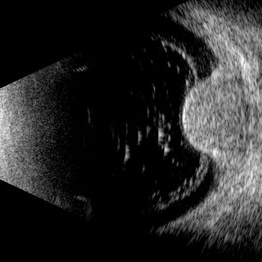 Choroidal Melanoma
Choroidal Melanoma
Jul 3 2025 by Gustavo Uriel Fonseca Aguirre
This B-mode transverse ultrasound scan shows asteroid hyalosis with partial posterior vitreous detachment. A dome-shaped choroidal melanoma is observed in the inferior quadrant (preequatorial to equatorial region), appearing as a solid, regularly bordered lesion with heterogeneous internal structure and mild acoustic attenuation. Standardized A-mode reveals medium-to-low internal reflectivity. The tumor measures 11.62 mm in base diameter and 6.60 mm in height. The retina and choroid remain attached, with minimal suprachoroidal fluid in the inferior quadrant.
Photographer: Gustavo U. Fonseca Aguirre, Hospital Conde de Valenciana, Ciudad de México
Condition/keywords: choroidal melanoma
-
 Evolving Weiss Ring
Evolving Weiss Ring
Sep 11 2022 by Michael B Green, MD, MBA
Fundus photograph of a 62-year-old female with an evolving Weiss-ring in the process of separating from the optic disc.
Condition/keywords: posterior vitreous detachment, PVD, Weiss ring
-
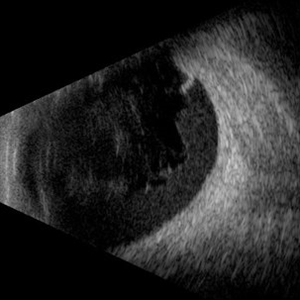 Hemorrhagic Vitreous Detachment
Hemorrhagic Vitreous Detachment
May 21 2025 by Gustavo Uriel Fonseca Aguirre
This B-mode longitudinal ultrasound scan shows a hemorrhagic vitreous detachment with the peripheral hyaloid strongly adherent to a retinal break. Associated vitreous and subhyaloid hemorrhage are present, indicating acute vitreoretinal traction.
Photographer: Gustavo U. Fonseca Aguirre, Hospital Conde de Valenciana, Ciudad de México
Condition/keywords: Hemorrhagic Vitreous Detachment
-
 Inactive Toxoplasmosis
Inactive Toxoplasmosis
Nov 9 2012 by Norman Byer
This is the same case as in the previous photograph showing the very large free operculum torn from the retina.
Condition/keywords: acute posterior vitreous detachment, free operculum, inactive toxoplasmosis, tractional retinal tear
-
 IOL Drop
IOL Drop
Dec 4 2025 by Surabhi Gupta, MS, DNB, FVRS
A 60 year old man presented with sudden dimunition of vision in right eye. His visual acuity was finger counting at 1 meter and best corrected visual acuity with +10 D was 6/9. Patient was diagnosed with spontaneous right eye IOL bag complex drop in vitreous cavity with superior HST and inferotemporal hole secondary to posterior vitreous detachment . Right eye montage color fundus photo shows rigid IOL bag complex in vitreous cavity with barraged superior HST and inferotemporal hole. Post barrage laser patient underwent pars plana vitrectomy with IOL explantation and scleral fixated IOL.
Photographer: Dr Surabhi Gupta
Imaging device: EDION FA
Condition/keywords: IOL drop
-
 Lattice Degeneration
Lattice Degeneration
Nov 9 2012 by Norman Byer
Lattice degeneration in a 42-year-old man which has produced four atrophic holes in a linear arrangement surrounded by a subclinical retinal detachment of unknown duration. By age 63, 21 years later, a posterior vitreous detachment was diagnosed in this eye, which was not present four years earlier. Nevertheless, the appearance seen here has remained exactly the same for 30 years, more than eight years with a concurrent PVD.
Condition/keywords: atrophic retinal hole, lattice degeneration, posterior vitreous detachment
-
 Lattice Lesion
Lattice Lesion
Nov 9 2012 by Norman Byer
This lattice lesion in a 44-year-old woman shows an interesting tuft arising from the edge of the lesion and seen well against the background of the shadow of the indentation. It is caused by glial proliferation into the vitreous condensation at the edge of the lesion. Around the borders of each lattice lesion there is an invariable attachment of condensed vitreous. It is this vitreoretinal attachment that comprises the chief danger of lattice lesions where it may lead to acute retinal tears and retinal detachment at the time of posterior vitreous detachment.
Condition/keywords: glial proliferation, lattice degeneration, scleral indentation, vitreoretinal attachment, vitreous condensation, white retinal tuft
-
Macular Hematoma Secondary Valsalva Maneuver
Oct 14 2021 by Islam bechakh
A 32-year-old man, who has presented for 02 months, a macular hematoma secondary to a Valsalva maneuver. He benefited from an attempt to open the hematoma with a Yag laser, but to no avail. We operated on and performed a 23G vitrectomy with posterior vitreous detachment, and discovered an epiretinal membrane which separated the hematoma from the posterior hyaloid. After removal of this membrane and aspiration of red blood cells and fibrin, the macula regained a normal appearance with good functional recovery.
Photographer: Islam Bechakh
Condition/keywords: epiretinal membrane (ERM), ERM, Macular hematoma, Valsalva maneuver
-
Morning-Glory-Syndrome
Dec 22 2017 by James B. Soque, CRA, OCT-C, COA, FOPS
68-year-old WM with Morning Glory Syndrome with PVD OS with Staphyloma surrounding optic nerve and extending into the macula. Also, esotropia OS from V1 nerve paresis from birth, with amblyopia.
Photographer: James B Soque, CRA OCT-C COA FOPS
Imaging device: Optos Daytona
Condition/keywords: color photo, esotropia, fundus photograph, Optomap, Optos, peripheral vascular disease (PVD), posterior vitreous detachment, staphyloma, ultra-wide field imaging, wide angle imaging
-
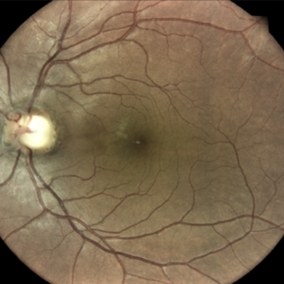
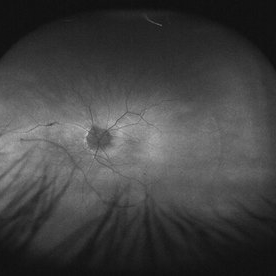 Myope With Staphyloma and Vitreous Detachment
Myope With Staphyloma and Vitreous Detachment
Jun 11 2016 by Philip J. Polkinghorne, MD
Fundus autofluorescence of a myope with PVD and staphyloma.
Imaging device: Optos FAF
Condition/keywords: degenerative myopia, myopia, staphyloma

 Loading…
Loading…