Search results (45 results)
-
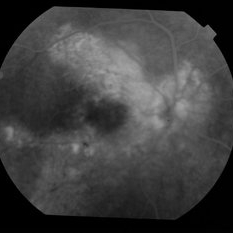
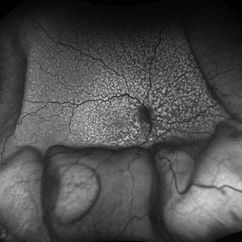 Idiopathic Uveal Effusion Syndrome
Idiopathic Uveal Effusion Syndrome
Aug 22 2024 by Jordyn Beckman
61 year old male with Idiopathic Uveal Effusion Syndrome with starry night appearance on fluorescein. 3 weeks s/p single external drainage retinotomy and 9 weeks of oral pred with recurrent choroidal effusions. Has since returned to surgery for secondary drainage retinotomy; subretinal fluid remain persistent.
Photographer: Jordyn Beckman
Imaging device: Optos California
Condition/keywords: chorioretinitis, Choroidal, exudative detachment, window defect
-
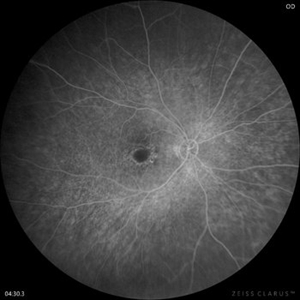 Flourescein Angiography of Cloroquine Toxicity
Flourescein Angiography of Cloroquine Toxicity
Feb 12 2024 by BENITO VERGARA, MD
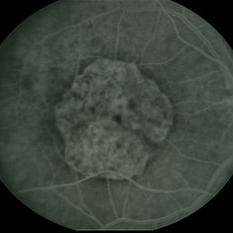
Image of a late phase fluorescein angiography at 4 minutes and 30 seconds of a 58-year-old woman treated with chloroquine at a daily dose of 3mg/kg, (recommended dose >2.3 mg/kg) that shows circular window defect suggestive of bullseye maculopathy.
Photographer: Benito Vergara Flores.
Imaging device: Clarus 700
Condition/keywords: chloroquine toxicity
-
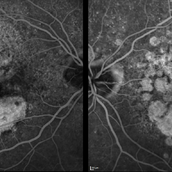 Macular Degeneration with Extensive Geographic Atrophy
Macular Degeneration with Extensive Geographic Atrophy
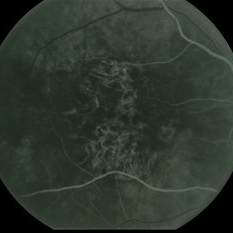
Jan 26 2022 by Olivia Rainey
Heidelberg Spectralis fluorescein angiography of a 94-year-old woman with Macular Degeneration affecting both eyes. The FA reveals transmission defects consistent with RPE changes and geographic atrophy of RPE of both eyes, as well as window defects consistent with peripheral scarring in the right eye. The patient's vision was Dcc20/70 in both eyes at the visit the images were taken.
Photographer: Olivia Rainey, OCT-C, COA
Imaging device: Heidelberg Spectralis
Condition/keywords: 30-degrees, choroidal neovascularization (CNV), dry age-related macular degeneration (dry AMD), early phase, fluorescein angiogram (FA), geographic atrophy, heidelberg spectralis, macular degeneration, neovascular age-related macular degeneration (AMD)
-
 PPCNVM and Peripheral Drusen Seen on Optos FA
PPCNVM and Peripheral Drusen Seen on Optos FA
Apr 22 2020 by John S. King, MD
72-year-old white male c/o of distortion OS for about 2 months. 20/100 OS, normotensive, small grey-green subretinal area just temporal to the optic disc. FA shows leakage c/w a ppcnvm; there is some SR and IR leakage as well as staining of peripheral drusen and some window defects from cobblestone. Avastin was adminstered.
Photographer: Asli Ahmed
Imaging device: CA
Condition/keywords: drusen, peripapillary choroidal neovascularization (PPCNVM)
-
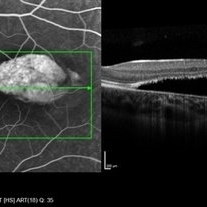 Torpedo Maculopathy
Torpedo Maculopathy
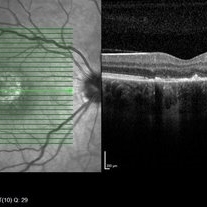
Jan 20 2020 by Pierre-Henry Gabrielle, MD
Coupled OCT B-scan and fluorescein angiogram of an asymptomatic 12-year-old girl with torpedo maculopathy of the left eye. One can report complete RPE atrophy at lesion site with window defect on FA and choroidal cavitation on OCT.
Photographer: Pierre-Henry Gabrielle, Ophthalmology department, Dijon University Hospital, France
Imaging device: Heidelberg Spectralis
Condition/keywords: fluorescein angiogram (FA), optical coherence tomography (OCT), torpedo maculopathy
-
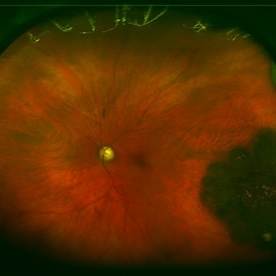
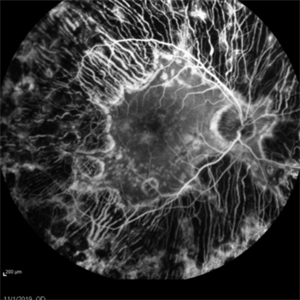 Enough PRP? (Proliferative Diabetic Retinopathy With Extreme PRP and Widespread Atrophy)
Enough PRP? (Proliferative Diabetic Retinopathy With Extreme PRP and Widespread Atrophy)
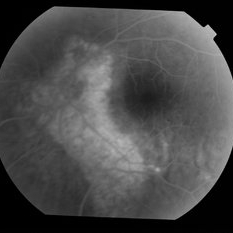
Nov 24 2019 by Thomas A. Ciulla, MD, MBA, FASRS
Fluorescein angiogram from a 71-year-old woman who underwent numerous sessions of pan retinal laser photocoagulation for proliferative diabetic retinopathy in the remote past. Note the widespread severe secondary atrophy, with only the central macular RPE remaining. Note the choroidal vessels through the diffuse window defect in the peripheral macula and near periphery.
Condition/keywords: laser injury, laser photocoagulation, proliferative diabetic retinopathy (PDR)
-
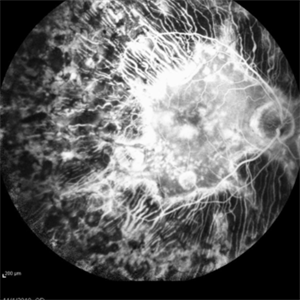 Enough PRP? (Proliferative Diabetic Retinopathy With Extreme PRP and Widespread Atrophy)
Enough PRP? (Proliferative Diabetic Retinopathy With Extreme PRP and Widespread Atrophy)
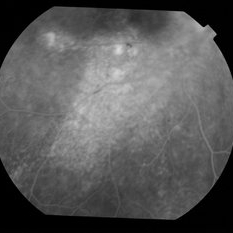
Nov 24 2019 by Thomas A. Ciulla, MD, MBA, FASRS
Fluorescein angiogram from a 71-year-old woman who underwent numerous sessions of pan retinal laser photocoagulation for proliferative diabetic retinopathy in the remote past. Note the widespread severe secondary atrophy, with only the central macular RPE remaining. Note the choroidal vessels through the diffuse window defect in the peripheral macula and near periphery.
Condition/keywords: laser injury, laser photocoagulation, proliferative diabetic retinopathy (PDR)
-
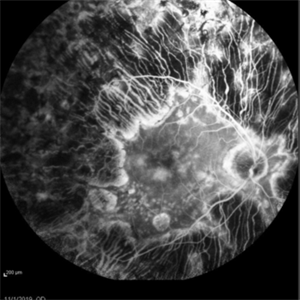 Enough PRP? (Proliferative Diabetic Retinopathy With Extreme PRP and Widespread Atrophy)
Enough PRP? (Proliferative Diabetic Retinopathy With Extreme PRP and Widespread Atrophy)
Nov 24 2019 by Thomas A. Ciulla, MD, MBA, FASRS
Fluorescein angiogram from a 71-year-old woman who underwent numerous sessions of pan retinal laser photocoagulation for proliferative diabetic retinopathy in the remote past. Note the widespread severe secondary atrophy, with only the central macular RPE remaining. Note the choroidal vessels through the diffuse window defect in the peripheral macula and near periphery.
Condition/keywords: laser injury, laser photocoagulation, proliferative diabetic retinopathy (PDR)
-
Unilateral Acute Idiopathic Maculopathy FA
May 7 2019 by William Ensor
A 37-year-old female presented with a two-week history of vision loss in the right eye. She experienced a flu-like illness including rash on the hands, feet, and mouth 2 days prior to her vision change. Her 3-year-old son had a similar illness diagnosed as hand, foot, and mouth disease by his pediatrician one week prior. Her visual acuity was 20/150 of the right eye, and 20/20 of the left eye. On dilated fundus examination, the left eye was unremarkable; the right eye revealed a circular, variably pigmented lesion of the macula. OCT imaging showed areas of RPE loss and clumping, with overlying loss of the photoreceptor layer. Fluorescein angiography showed central and peripheral hyperfluorescence consistent with window defect, and blockage in area of RPE loss. No treatment was initiated at this time. The patient returned 10 days later; her visual acuity improved to 20/50 in the right eye. Dilated fundus exam showed increased pigmentation of the macular lesion. OCT of the right eye showed further RPE clumping without recovery of the photoreceptor layer, despite her improved visual acuity.
Condition/keywords: unilateral acute idiopathic maculopathy
-
Unilateral Acute Idiopathic Maculopathy FA
May 7 2019 by William Ensor
A 37-year-old female presented with a two-week history of vision loss in the right eye. She experienced a flu-like illness including rash on the hands, feet, and mouth 2 days prior to her vision change. Her 3-year-old son had a similar illness diagnosed as hand, foot, and mouth disease by his pediatrician one week prior. Her visual acuity was 20/150 of the right eye, and 20/20 of the left eye. On dilated fundus examination, the left eye was unremarkable; the right eye revealed a circular, variably pigmented lesion of the macula. OCT imaging showed areas of RPE loss and clumping, with overlying loss of the photoreceptor layer. Fluorescein angiography showed central and peripheral hyperfluorescence consistent with window defect, and blockage in area of RPE loss. No treatment was initiated at this time. The patient returned 10 days later; her visual acuity improved to 20/50 in the right eye. Dilated fundus exam showed increased pigmentation of the macular lesion. OCT of the right eye showed further RPE clumping without recovery of the photoreceptor layer, despite her improved visual acuity.
Condition/keywords: unilateral acute idiopathic maculopathy
-
Unilateral Acute Idiopathic Maculopathy Fundus
May 7 2019 by William Ensor
A 37-year-old female presented with a two-week history of vision loss in the right eye. She experienced a flu-like illness including rash on the hands, feet, and mouth 2 days prior to her vision change. Her 3-year-old son had a similar illness diagnosed as hand, foot, and mouth disease by his pediatrician one week prior. Her visual acuity was 20/150 of the right eye, and 20/20 of the left eye. On dilated fundus examination, the left eye was unremarkable; the right eye revealed a circular, variably pigmented lesion of the macula. OCT imaging showed areas of RPE loss and clumping, with overlying loss of the photoreceptor layer. Fluorescein angiography showed central and peripheral hyperfluorescence consistent with window defect, and blockage in area of RPE loss. No treatment was initiated at this time. The patient returned 10 days later; her visual acuity improved to 20/50 in the right eye. Dilated fundus exam showed increased pigmentation of the macular lesion. OCT of the right eye showed further RPE clumping without recovery of the photoreceptor layer, despite her improved visual acuity.
Condition/keywords: unilateral acute idiopathic maculopathy
-
Unilateral Acute Idiopathic Maculopathy Fundus
May 7 2019 by William Ensor
A 37-year-old female presented with a two-week history of vision loss in the right eye. She experienced a flu-like illness including rash on the hands, feet, and mouth 2 days prior to her vision change. Her 3-year-old son had a similar illness diagnosed as hand, foot, and mouth disease by his pediatrician one week prior. Her visual acuity was 20/150 of the right eye, and 20/20 of the left eye. On dilated fundus examination, the left eye was unremarkable; the right eye revealed a circular, variably pigmented lesion of the macula. OCT imaging showed areas of RPE loss and clumping, with overlying loss of the photoreceptor layer. Fluorescein angiography showed central and peripheral hyperfluorescence consistent with window defect, and blockage in area of RPE loss. No treatment was initiated at this time. The patient returned 10 days later; her visual acuity improved to 20/50 in the right eye. Dilated fundus exam showed increased pigmentation of the macular lesion. OCT of the right eye showed further RPE clumping without recovery of the photoreceptor layer, despite her improved visual acuity.
Condition/keywords: unilateral acute idiopathic maculopathy
-
Unilateral Acute Idiopathic Maculopathy Fundus
May 7 2019 by William Ensor
A 37-year-old female presented with a two-week history of vision loss in the right eye. She experienced a flu-like illness including rash on the hands, feet, and mouth 2 days prior to her vision change. Her 3-year-old son had a similar illness diagnosed as hand, foot, and mouth disease by his pediatrician one week prior. Her visual acuity was 20/150 of the right eye, and 20/20 of the left eye. On dilated fundus examination, the left eye was unremarkable; the right eye revealed a circular, variably pigmented lesion of the macula. OCT imaging showed areas of RPE loss and clumping, with overlying loss of the photoreceptor layer. Fluorescein angiography showed central and peripheral hyperfluorescence consistent with window defect, and blockage in area of RPE loss. No treatment was initiated at this time. The patient returned 10 days later; her visual acuity improved to 20/50 in the right eye. Dilated fundus exam showed increased pigmentation of the macular lesion. OCT of the right eye showed further RPE clumping without recovery of the photoreceptor layer, despite her improved visual acuity.
Condition/keywords: unilateral acute idiopathic maculopathy
-
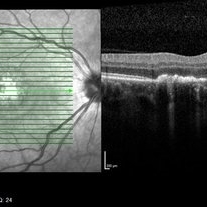 Unilateral Acute Idiopathic Maculopathy OCT Macula
Unilateral Acute Idiopathic Maculopathy OCT Macula
May 7 2019 by William Ensor
A 37-year-old female presented with a two-week history of vision loss in the right eye. She experienced a flu-like illness including rash on the hands, feet, and mouth 2 days prior to her vision change. Her 3-year-old son had a similar illness diagnosed as hand, foot, and mouth disease by his pediatrician one week prior. Her visual acuity was 20/150 of the right eye, and 20/20 of the left eye. On dilated fundus examination, the left eye was unremarkable; the right eye revealed a circular, variably pigmented lesion of the macula. OCT imaging showed areas of RPE loss and clumping, with overlying loss of the photoreceptor layer. Fluorescein angiography showed central and peripheral hyperfluorescence consistent with window defect, and blockage in area of RPE loss. No treatment was initiated at this time. The patient returned 10 days later; her visual acuity improved to 20/50 in the right eye. Dilated fundus exam showed increased pigmentation of the macular lesion. OCT of the right eye showed further RPE clumping without recovery of the photoreceptor layer, despite her improved visual acuity.
Condition/keywords: unilateral acute idiopathic maculopathy
-
 Unilateral Acute Idiopathic Maculopathy OCT Macula
Unilateral Acute Idiopathic Maculopathy OCT Macula
May 7 2019 by William Ensor
A 37-year-old female presented with a two-week history of vision loss in the right eye. She experienced a flu-like illness including rash on the hands, feet, and mouth 2 days prior to her vision change. Her 3-year-old son had a similar illness diagnosed as hand, foot, and mouth disease by his pediatrician one week prior. Her visual acuity was 20/150 of the right eye, and 20/20 of the left eye. On dilated fundus examination, the left eye was unremarkable; the right eye revealed a circular, variably pigmented lesion of the macula. OCT imaging showed areas of RPE loss and clumping, with overlying loss of the photoreceptor layer. Fluorescein angiography showed central and peripheral hyperfluorescence consistent with window defect, and blockage in area of RPE loss. No treatment was initiated at this time. The patient returned 10 days later; her visual acuity improved to 20/50 in the right eye. Dilated fundus exam showed increased pigmentation of the macular lesion. OCT of the right eye showed further RPE clumping without recovery of the photoreceptor layer, despite her improved visual acuity.
Condition/keywords: unilateral acute idiopathic maculopathy
-
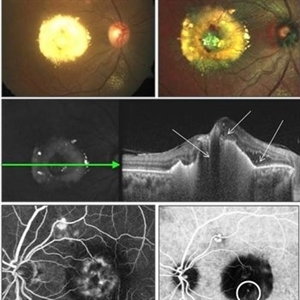 Polypoidal Chroidal Vasculopathy
Polypoidal Chroidal Vasculopathy
Sep 21 2018 by Dhaivat Shah
A 40-year-old female presented with sudden onset decreased vision in right eye. BCVA: CF 1 mt. Fundus showed massive subretinal exudation with haemorrhage. EDI OCT showed notched PEDs with shallow SRF and exudation with back-shadowing. FFA shows leak with window defects. ICG shows hotspot in late phase. Polypoidal choroidal vasculopathy (PCV) is a retinal disorder characterized by the presence of aneurysmal polypoidal lesions in the choroidal vasculature, resulting in damage to the overlying retina and loss of retinal pigment epithelium. The aneurysmal dilatations, also known as polyps, may be found subfoveal, juxtafoveal, extrafoveal, peripapillary or even peripheral regions. The polypoidal lesions are best detected on indocyanine green angiography as hotspots in late phase. The presence of choroidal polyps can lead to recurrent episodes of exudative retinal detachment, serous or hemorrhagic pigment epithelial detachment, subretinal hemorrhage and exudation. Treatment is available in form of laser/PDT along with Anti VEGF injection.
Photographer: Miss Moupiya Das
Condition/keywords: polypoidal choroidal vasculopathy (PCV)
-
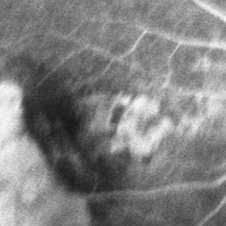
 Adenocarcinoma Arising from CHRPE
Adenocarcinoma Arising from CHRPE
Sep 17 2015 by Marc C. Peden, MD
49-year-old female referred for presumed ocular melanoma. On examination was noted to have darkly pigmented lesion in the temporal retina of left eye. Lesion had characteristic scalloped edges with central lacunae, however, on ultrasonography was noted to have 1.8mm of elevation with high internal reflectivity. IVFA shows absence of dual circulation with areas of window defect. Findings were consistent with those described by Shields et al., in their April 2001 article in Archives of Ophthalmology.
Photographer: Janet Traynom COT
Imaging device: Optos P200MA
Condition/keywords: adenocarcinoma arising from CHRPE
-
 Adenocarcinoma Arising from CHRPE
Adenocarcinoma Arising from CHRPE
Sep 17 2015 by Marc C. Peden, MD
49-year-old female referred for presumed ocular melanoma. On examination was noted to have darkly pigmented lesion in the temporal retina of left eye. Lesion had characteristic scalloped edges with central lacunae, however, on ultrasonography was noted to have 1.8mm of elevation with high internal reflectivity. IVFA shows absence of dual circulation with areas of window defect. Findings were consistent with those described by Shields et al., in their April 2001 article in Archives of Ophthalmology.
Photographer: Janet Traynom
Imaging device: Optos P200MA
Condition/keywords: adenocarcinoma arising from CHRPE
-
 RPE Tear: Fluorescein Angiography
RPE Tear: Fluorescein Angiography
May 2 2015 by Thomas A. Ciulla, MD, MBA, FASRS
Mid Phase Fluorescein Angiogram: The scrolled and redundant RPE just temporal to the fovea blocks underlying choroidal fluorescence. The absent RPE, more temporally, results in a window defect with intense hyperfluorescence.
Photographer: Stuart Alfred
Condition/keywords: choroidal neovascular membrane (CNVM), retinal pigment epithelium (RPE) tear, wet age-related macular degeneration (wet AMD)
-
 FA After Thermal Laser for CNVM
FA After Thermal Laser for CNVM
Feb 19 2015 by H. Michael Lambert, MD
AV phase of fluorescein angiogram with RPE window defect after thermal laser.
Condition/keywords: choroidal neovascular membrane (CNVM), laser, window defect
-
 Central Areolar Choroidal Dystrophy
Central Areolar Choroidal Dystrophy
Jan 5 2015 by H. Michael Lambert, MD
Later fluorescein angiogram OD with central, well defined, confluent atrophy, window defect with transmission.
Condition/keywords: central areolar choroidal dystrophy (CACD)
-
 Central Areolar Choroidal Dystrophy
Central Areolar Choroidal Dystrophy
Jan 5 2015 by H. Michael Lambert, MD
Early fluorescein angiogram OD with central, well defined, confluent atrophy, window defect with choroidal vessels visible.
Condition/keywords: central areolar choroidal dystrophy (CACD)
-
 Chronic CSCR Resolution With Anti-VEGF
Chronic CSCR Resolution With Anti-VEGF
Jul 31 2014 by Mallika Goyal, MD
Fluorescein of the left eye of a 55-year-old male who presented with fellow eye symptoms from chronic CSCR (> 3 years) shows extensive RPE window defects.
Photographer: Mallika Goyal, MD, Apollo Health City, Jubilee Hills, Hyderabad-500033
Condition/keywords: chronic central serous chorioretinopathy (CSCR)
-
 Chronic CSCR Resolution With Anti-VEGF
Chronic CSCR Resolution With Anti-VEGF
Jul 31 2014 by Mallika Goyal, MD
Fluorescein of the inferior fundus of the right eye of a 55-year-old male who presented with symptoms from chronic CSCR (> 3 years) shows extensive RPE window defects and occasional areas of intense hyperfluorescence.
Photographer: Mallika Goyal, MD, Apollo Health City, Jubilee Hills, Hyderabad-500033
Condition/keywords: chronic central serous chorioretinopathy (CSCR)
-
 Chronic CSCR Resolution With Anti-VEGF
Chronic CSCR Resolution With Anti-VEGF
Jul 31 2014 by Mallika Goyal, MD
Fluorescein of the right eye of a 55-year-old male who presented with symptoms from chronic CSCR (> 3 years) shows extensive RPE window defects and occasional areas of intense hyperfluorescence.
Photographer: Mallika Goyal, MD, Apollo Health City, Jubilee Hills, Hyderabad-500033
Condition/keywords: chronic central serous chorioretinopathy (CSCR)

 Loading…
Loading…