Search results (90 results)
-
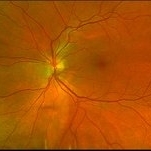
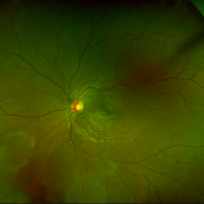
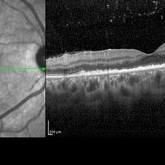 Posterior Placoid Chorioretinitis
Posterior Placoid Chorioretinitis
Mar 9 2025 by Oscar Francisco Miranda, MD
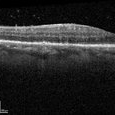
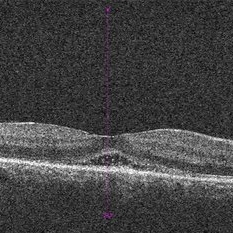
A 36-year-old male with bilateral visual loss of 3 months' duration, with no relevant medical history on inquiry. A round-shaped lesion with well-defined borders and a yellowish-white color is observed in the macula of both eyes, accompanied by vitreous cellularity. The macular OCT shows a dentate RPE. The VDRL, FTA-ABS, and HIV tests were positive.
Photographer: Oscar Francisco Miranda-Gómez
Imaging device: Heidelberg Spectralis
Condition/keywords: acute syphilitic posterior placoid chorioretinitis, OCT, Ocular syphilis
-
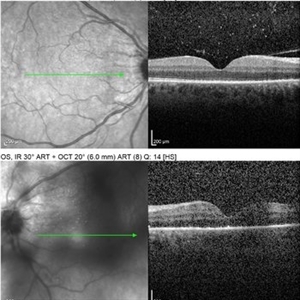
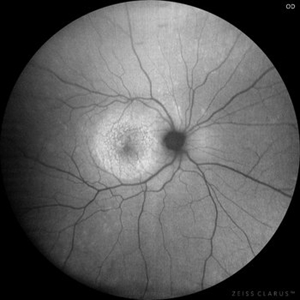 Posterior Placoid Chorioretinitis
Posterior Placoid Chorioretinitis
Mar 9 2025 by Oscar Francisco Miranda, MD
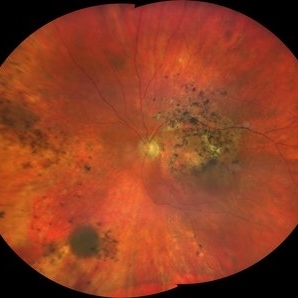
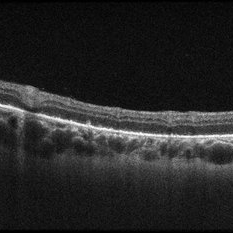
A 36-year-old male with bilateral visual loss of 3 months' duration, with no relevant medical history on inquiry. A round-shaped lesion with well-defined borders and a yellowish-white color is observed in the macula of both eyes, accompanied by vitreous cellularity. The macular OCT shows a dentate RPE. The VDRL, FTA-ABS, and HIV tests were positive.
Photographer: Oscar Francisco Miranda-Gómez
Imaging device: Autofluorescence Zeiss Clarus 700
Condition/keywords: acute posterior placoid chorioretinitis, Autofluorescence, ocular syphilis
-
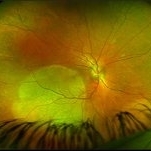
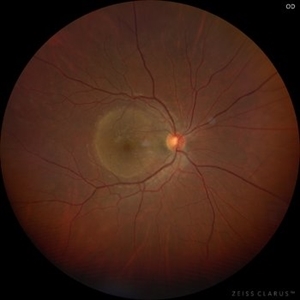 Posterior Placoid Chorioretinitis
Posterior Placoid Chorioretinitis
Mar 9 2025 by Oscar Francisco Miranda, MD
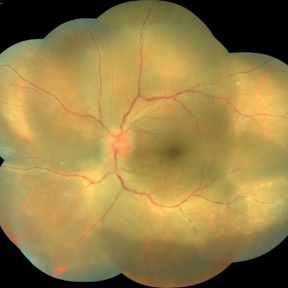
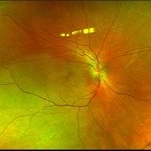
A 36-year-old male with bilateral visual loss of 3 months' duration, with no relevant medical history on inquiry. A round-shaped lesion with well-defined borders and a yellowish-white color is observed in the macula of both eyes, accompanied by vitreous cellularity. The macular OCT shows a dentate RPE. The VDRL, FTA-ABS, and HIV tests were positive.
Photographer: Oscar Francisco Miranda-Gómez
Imaging device: Zeiss Clarus 700
Condition/keywords: acute posterior placoid chorioretinitis, Ocular syphilis
-
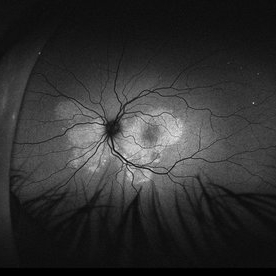
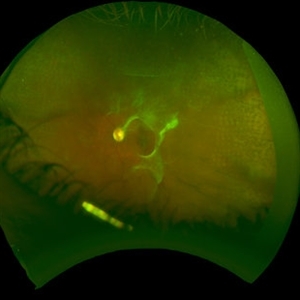
 Acute Syphilitic Posterior Placoid Chorioretinitis
Acute Syphilitic Posterior Placoid Chorioretinitis
Oct 20 2024 by César Adrián Gómez Valdivia, MD
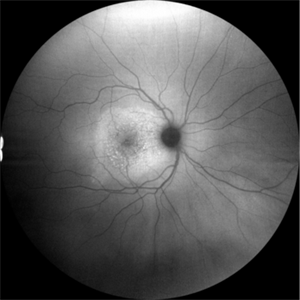
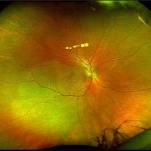
Fundus autofluorescence image of an acute syphilitic posterior placoid chorioretinitis found in a HIV positive 28 YO male patient with suspected neurosyphilis. A beautiful butterfly autofluorescence pattern can be appreciated.
Photographer: @eyemissu2
Imaging device: California ICG OPTOS
Condition/keywords: acute syphilitic posterior placoid chorioretinitis
-
 Acute Syphilitic Posterior Placoid Chorioretinitis
Acute Syphilitic Posterior Placoid Chorioretinitis
Oct 16 2024 by César Adrián Gómez Valdivia, MD
Fundus autofluorescence image of an acute syphilitic posterior placoid chorioretinitis found in a HIV positive 28 YO male patient with suspected neurosyphilis. A beautiful butterfly autofluorescence pattern can be appreciated.
Photographer: @eyemissu2
Imaging device: California ICG OPTOS
Condition/keywords: acute syphilitic posterior placoid chorioretinitis, chorioretinitis, syphilis
-
 Ocular Syphilis
Ocular Syphilis
Feb 21 2024 by Nikhil K Bommakanti, MD
A monocular man in his sixties presented with blurred vision in the right eye for two months. Optical coherence tomography demonstrated vitreous cells and characteristic inflammatory deposits of the outer retina and retinal pigment epithelium, and laboratory testing confirmed the diagnosis of syphilis. He was admitted for intravenous penicillin and consultation with a specialist in infectious diseases.
Condition/keywords: syphilis
-
 Healed Syphilitic Retinitis
Healed Syphilitic Retinitis
Aug 2 2023 by Kamal Kishore, MD, MBBS
A 54-year-old male with treated syphilitic retinitis left eye.
Photographer: Tanya Huston, COA
Imaging device: Zeiss Clarus
Condition/keywords: syphilis
-
 Syphilitic Uveitis
Syphilitic Uveitis
May 26 2023 by Virginia Gebhart
35-year-old female with resolved syphilitic uveitis OU. Severe retinal thinning with chalky ON pallor and severe vessel attenuation associated with presumed post syphilitic neuritis vs bilateral CRAO's in both eyes. Pt reports acute bilateral vision loss after delivery of her child in 8/2021. Limited VA OU due to severe optic nerve and macula atrophy.
Photographer: Virginia Gebhart, Retina Consultants of Carolina
Imaging device: Topcon TRC 50DX
Condition/keywords: syphilis, uveitis
-
Exudation in peripapillary retina due to syphilis
Mar 9 2023 by Sergio Ivan Escamilla
Left eye fundus photograph of 51-year-old male with peripapillary exudation due to syphilis confirmed by FTA ABS and VDRL with high nontreponemal antibody titers
Photographer: Ivan Escamilla, Hospital Central Militar, Cd. Mexico.
Imaging device: claurus 700
Condition/keywords: syphilis
-
 Acute syphilitic posterior placoid chorioretinitis
Acute syphilitic posterior placoid chorioretinitis
Apr 24 2022 by Aniruddha K Agarwal, MD
Green-light fundus autofluorescence (FAF) of the right eye from a 55-year-old man with risk factors for sexually trasnmitted diseases who presented to the retina clinic for a central scotoma. Funduscopy revealed a placoid lesion in the posterior pole. FAF highlights a hyperautofluorescent placoid lesion involving the macula with granular hyperfluorescence. The patient tested positive for syphilis and received intravenous penicillin treatment.
Photographer: Esther CIANCAS, MD, PhD, Gema CRESPO-RODRÍGUEZ, RN
Imaging device: Zeiss Clarus fundus camera
Condition/keywords: chorioretinitis, IUSG, syphilis, uveitis
-
 Acute Syphilitic Posterior Placoid Chorioretinitis (ASPPC)
Acute Syphilitic Posterior Placoid Chorioretinitis (ASPPC)
May 12 2021 by Joseph D Boss, MD
Ultra-widefield fundus photograph of a 36-year-old male with acute syphilitic posterior placoid chorioretinitis. Subsequent testing reviewed a positive RPR 1:256 and positive syphilis antibody.
Photographer: Joseph Boss, MD; Retina Specialists of Michigan
Condition/keywords: acute syphilitic posterior placoid chorioretinitis, syphilitis uveitis
-
 Acute Syphilitic Posterior Placoid Chorioretinitis with Papillitis
Acute Syphilitic Posterior Placoid Chorioretinitis with Papillitis
Mar 30 2021 by Tanya Jain
A 41-year-old homosexual male patient presented with placoid chorioretinitis and was diagnosed with acute syphilitic posterior placoid chorioretinitis, neurosyphilis and HIV disease. The patient was started with HAART and intravenous antibiotics.
Photographer: Tanya Jain
Condition/keywords: acute syphilitic posterior placoid chorioretinitis, choroiditis, papillitis
-
 Palms of Patient with Placoid Lesions in Posterior Segment
Palms of Patient with Placoid Lesions in Posterior Segment
Dec 20 2020 by John S. King, MD
44-year-old white female seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), Plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU. Va 20/200 OD and 20/20 OS, IOP 12 OU, Pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery. There was trace vitreous cell OS, mild disc edema, and a large, granular placoid area nasally that appeared to be granulated. The OCT showed mild subfoveal fluid with nodular areas in the RPE and some overlying irregular architecture of the outer retina. Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand (See Image), and later learned that she had a rash on the soles of her feet. She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started). She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated. OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer.
Imaging device: Optos CA
Condition/keywords: acute syphilitic posterior placoid chorioretinitis
-
 Posterior Placoid Chorioretinopathy
Posterior Placoid Chorioretinopathy
Dec 19 2020 by John S. King, MD
44-year-old white female seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU. Va 20/200 OD and 20/20 OS, IOP 12 OU, pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery. There was a trace vitreous cell OS with a large, granular placoid lesion nasally. The OCT (see above) shows mild subfoveal fluid with nodular areas in the RPE and some overlying irregular architecture of the outer retina. Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand, and later learned that she had a rash on the soles of her feet. She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started). She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated. OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer.
Imaging device: Zeiss Cirrus
Condition/keywords: acute syphilitic posterior placoid chorioretinitis, syphilis
-
 Posterior Placoid Chorioretinopathy
Posterior Placoid Chorioretinopathy
Dec 19 2020 by John S. King, MD
44-year-old white female seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU. Va 20/200 OD and 20/20 OS, IOP 12 OU, pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery. There was a trace vitreous cell OS with a large, granular placoid lesion nasally. The OCT via the lesion (see above) shows nodular areas in the RPE and some overlying disruption of EZ and outer retina. Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand, and later learned that she had a rash on the soles of her feet. She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started). She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated. OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer.
Imaging device: Zeiss Cirrus
Condition/keywords: acute syphilitic posterior placoid chorioretinitis, syphilis
-
 Posterior Placoid Chorioretinopathy
Posterior Placoid Chorioretinopathy
Dec 19 2020 by John S. King, MD
44-year-old white female seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU. Va 20/200 OD and 20/20 OS, IOP 12 OU, pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery. There was trace vitreous cell OS, mild disc edema, and a large, granular placoid area nasally that appeared to be granulated. The OCT showed mild subfoveal fluid with nodular areas in the RPE and some overlying irregular architecture of the outer retina. Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand, and later learned that she had a rash on the soles of her feet. She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started). She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated (See Image). OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer.
Photographer: Ashley Seiger
Imaging device: Optos CA
Condition/keywords: acute syphilitic posterior placoid chorioretinitis
-
 Posterior Placoid Chorioretinopathy
Posterior Placoid Chorioretinopathy
Dec 19 2020 by John S. King, MD
44-year-old white female seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU. Va 20/200 OD and 20/20 OS, IOP 12 OU, pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery. There was trace vitreous cell OS, mild disc edema, and a large, granular placoid area nasally that appeared to be granulated. The OCT showed mild subfoveal fluid with nodular areas in the RPE and some overlying irregular architecture of the outer retina. Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand, and later learned that she had a rash on the soles of her feet. She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started). She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated (See Image). OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer.
Photographer: Ashley Seiger
Imaging device: Optos CA
Condition/keywords: acute syphilitic posterior placoid chorioretinitis, syphilis
-
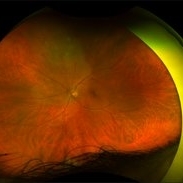
 Syphilis Placoid Initial Image OS
Syphilis Placoid Initial Image OS
Dec 19 2020 by John S. King, MD
44-year-old white female seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU. Va 20/200 OD and 20/20 OS, IOP 12 OU, pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery. There was trace vitreous cell OS, mild disc edema, and a large, granular placoid area nasally that appeared to be granulated (See Image). The OCT showed mild subfoveal fluid with nodular areas in the RPE and some overlying irregular architecture of the outer retina. Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand, and later learned that she had a rash on the soles of her feet. She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started).... She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated. OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer.
Imaging device: Optos CA
Condition/keywords: acute syphilitic posterior placoid chorioretinitis, syphilis
-
 Posterior Placoid Chorioretinopathy
Posterior Placoid Chorioretinopathy
Dec 19 2020 by John S. King, MD
44-year-old white female seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), Plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU. Va 20/200 OD and 20/20 OS, IOP 12 OU, pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery, and two possible smaller spots SN (See Photo above). There was a trace vitreous cell OS with a large, granular placoid lesion nasally. The OCT showed mild subfoveal fluid with nodular areas in the RPE and some overlying irregular architecture of the outer retina. Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand, and later learned that she had a rash on the soles of her feet. She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started). She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated. OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer.
Imaging device: Optos CA
Condition/keywords: acute syphilitic posterior placoid chorioretinitis, syphilis
-
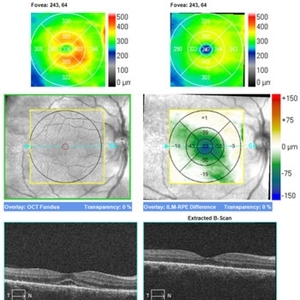 Posterior Placoid Chorioretinopathy
Posterior Placoid Chorioretinopathy
Dec 19 2020 by John S. King, MD
44-year-old white female seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU. Va 20/200 OD and 20/20 OS, IOP 12 OU, Pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery. There was trace vitreous cell OS, mild disc edema, and a large, granular placoid area nasally that appeared to be granulated. The OCT showed mild subfoveal fluid with nodular areas in the RPE and some overlying irregular architecture of the outer retina. Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand, and later learned that she had a rash on the soles of her feet. She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started). She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated. OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer (See Image).
Imaging device: Zeiss Cirrus
Condition/keywords: acute syphilitic posterior placoid chorioretinitis, syphilis
-
 Acute Syphilitic Posterior Placoid Chorioretinitis
Acute Syphilitic Posterior Placoid Chorioretinitis
Nov 22 2020 by Shawn Sell
58-year-old homeless male presenting with 2 weeks of bilateral eye redness and photosensitivity found to have panuveitis with a positive VDRL CSF and RPR titer of 1:512 with acute syphilitic posterior placoid chorioretinitis.
Photographer: Eastern Virginia Medical School
Imaging device: Optos
Condition/keywords: acute syphilitic posterior placoid chorioretinitis, neurosyphilis
-
 Syphilitic Chorioretinitis
Syphilitic Chorioretinitis
Oct 2 2020 by David L Kilpatrick, MD
22-year-old female presented with painless blurry vision OD > OS for one week. On exam, she exhibited moderate vitritis, papillitis and broad placoid chorioretinitis OD and multifocal placoid peripheral chorioretinitis OS (without vitritis or papillitis). The anterior segment was unremarkable OU. Serum RPR and confirmatory treponemal Ab were both positive. Neuroimaging and CSF studies were unremarkable. A 2 week course of IV penicillin was initiated. The placoid lesions had resolved five days after beginning treatment.
Photographer: Mississippi Retina Associates
Condition/keywords: acute syphilitic posterior placoid chorioretinitis, syphilis
-
 Neurosyphilis
Neurosyphilis
Sep 3 2020 by Ankur S. Gupta, MD, MS
40-year-old male who presented with blurry vision and hand lesions. Hyperreflective nodularity of the retinal pigment epithelium overlying loss of the normal photoreceptor architecture. Disruption of the external limiting membrane. Loss of the photoreceptor inner segment/outer segment band. Punctate hyperfluorescence in the choroid. Transient subretinal fluid.
Photographer: Kenneth Lam; Geisinger Eye Institute
Condition/keywords: neurosyphilis, uveitis
-
 Eales Disease Causing TRD and Macular Edema in Pregnancy
Eales Disease Causing TRD and Macular Edema in Pregnancy
Apr 21 2020 by Richard M Martindale, MD
42-year-old pregnant African American with TRD and peripheral ischemia secondary to Eales disease. She was assigned this diagnosis of exclusion after a thorough work up for other identifiable causes of peripheral ischemia (e.g. sickle cell, syphilis, sarcoid, clotting disorders, SLE, TB, IP, FEVR). We elected to temporize her with PRP and Ozurdex in lieu of anti-VEGF medication given her pregnant status. Note: the Ozurdex pellet is visible in the inferior aspect of this photo.
Photographer: Retina Consultants of Alabama
Imaging device: Optos
Condition/keywords: Eales disease
-
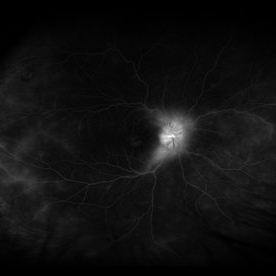 Syphilitic Uveitis
Syphilitic Uveitis
Apr 2 2020 by Olivia Rainey
Ultrawide-field fluorescein angiogram of a 42-year-old male with syphilitic uveitis affecting his right eye more than his left. Patient is HIV positive. He developed hearing loss and palm/leg/scalp rash prompting diagnosis of neurosyphilis, s/p IM and full IV course of 2.4 Mil PCN G, and finished this course 3/9/20. He admits to recent rectal bleeding with ongoing plan for colonoscopy 3/16/20. He has a history of extensive travel including London, Hong Kong, and Bangkok. His husband has also been treated with IV PCN G, however per chart review he has multiple sexual partners. Patient's vision was 20/20 in each eye.
Photographer: Olivia Rainey
Imaging device: Optos California
Condition/keywords: disc hyperfluorescence, FA late phase leakage, fluorescein angiogram (FA), fluorescein leakage, HIV, late phase, optic nerve edema, Optos, phelbitis, syphilis neuroretinopathy, ultra-wide field imaging, uveitis

 Loading…
Loading…