Search results (155 results)
-
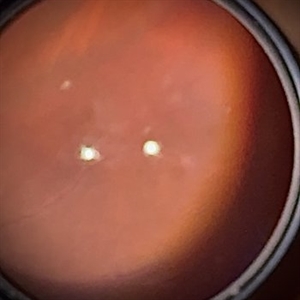 Kyrieleis Plaques
Kyrieleis Plaques
Aug 18 2025 by Helder Vasconcelos
Kyrieleis Plaques and vitritis in a patient with posterior uveitis secondary to presumed ocular toxoplasmosis.
Photographer: Helder Vasconcelos
Imaging device: Smartphone Fundoscopy
Condition/keywords: kyrieleis plaques, toxoplasmosis chorioretinitis
-
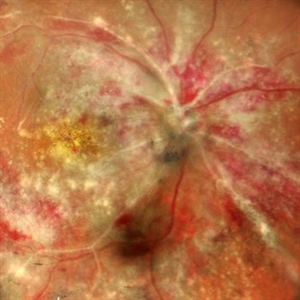
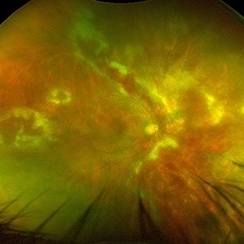
 CMV Retinitis: Turning Retina into Abstract Art Since Immunosuppression
CMV Retinitis: Turning Retina into Abstract Art Since Immunosuppression
Aug 4 2025 by rohan jain
We report a case of 34 years old HIV positive male who presented with Diminution of vision in OD since 1 month .Examination of OD showed hazy media due to vitritis, diffuse yellowish-whitish retinal necrosis and retinal hemorrhages around the disc and attenuated retinal vessels.
Photographer: Dr. ROHAN JAIN
Imaging device: mirante
Condition/keywords: CMV chorioretinitis, CMV retinitis, cytomegalovirus (CMV), Cytomegalovirus Retinitis
-
 CMV Retinitis: Turning Retina into Abstract Art Since Immunosuppression
CMV Retinitis: Turning Retina into Abstract Art Since Immunosuppression
Aug 4 2025 by rohan jain
We report a case of 34 years old HIV positive male who presented with Diminution of vision in OD since 1 month. Examination of OD showed hazy media due to vitritis, diffuse yellowish-whitish retinal necrosis and retinal hemorrhages around the disc and attenuated retinal vessels.
Photographer: Dr. ROHAN JAIN
Imaging device: mirante
Condition/keywords: CMV chorioretinitis, CMV retinitis, cytomegalovirus (CMV), Cytomegalovirus Retinitis
-
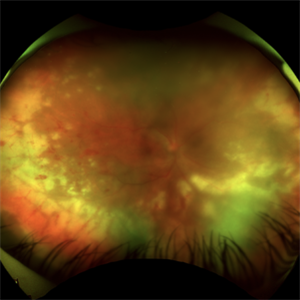 Acute Retinal Necrosis
Acute Retinal Necrosis
Jul 3 2025 by Heitor Nogueira
Fundus photograph of an 53-year-old woman with patient who reported unilateral visual acuity loss for 10 days associated with ocular pain. She presented conjunctival hyperemia with temporal and nasal nodular scleritis, anterior chamber reaction 2+/4+, Koeppe nodules, granulomatous PKs, vitritis 2+/4+, multiple areas of vasculitis in arcades and periphery, associated with hemorrhages and necrotizing retinitis in temporal, inferior and nasal periphery. patient who reported unilateral visual acuity loss for 10 days associated with ocular pain. He presented conjunctival hyperemia with temporal and nasal nodular scleritis, anterior chamber reaction 2+/4+, Koeppe nodules, granulomatous PKs, vitreitis 2+/4+, multiple areas of vasculitis in the arcades and periphery, associated with hemorrhages and necrotizing retinitis in the temporal, inferior and nasal periphery. Positive serology for Herpes Virus.
Photographer: Heitor Nogueira, Penido Burnier Institute and CHOV, Campinas, São Paulo, Brazil
Imaging device: Optos Daytona
Condition/keywords: ARN complications, Herpes, progressive outer retinal necrosis (PORN)
-
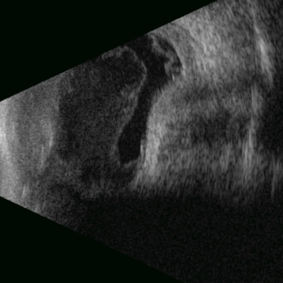 Posterior Nodular Scleritis
Posterior Nodular Scleritis
Apr 23 2025 by Gustavo Uriel Fonseca Aguirre
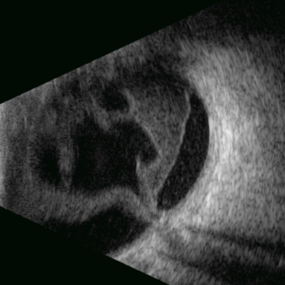
This B-mode ultrasound scan demonstrates a posterior scleral nodule accompanied by vitritis, serous retinal detachment, and annular choroidal detachment. The nodule appears as a localized hypoechoic scleral thickening, while the serous retinal detachment shows a smooth convex configuration. The choroidal detachment presents with the characteristic ring-shaped elevation, suggesting significant intraocular inflammation or hypotony.
Photographer: Gustavo U. Fonseca Aguirre, Hospital Conde de Valenciana, Ciudad de México
Condition/keywords: posterior nodular scleritis, posterior scleritis
-
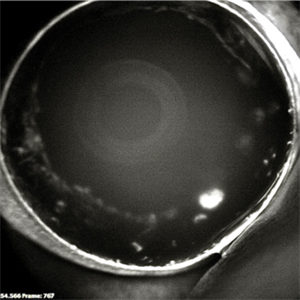
 Stag Horn
Stag Horn
Apr 8 2025 by Gustavo Uriel Fonseca Aguirre
B-mode ultrasound of a young male patient with bilateral panuveitis (currently under investigation) reveals intense vitritis with islands of preserved vitreous and partial posterior hyaloid detachment, creating a characteristic "stag horn" appearance.
Photographer: Gustavo U. Fonseca Aguirre, Hospital Conde de Valenciana, Ciudad de México
Condition/keywords: Panuveitis
-
 Post Dengue Fever Retinitis
Post Dengue Fever Retinitis
Dec 27 2024 by Tejaswita Verma
A 35 year old female presented with bilaterally decreased vision since a month post dengue fever. Vision was finger counting 6 mt. in the RE and 6/36 in the left eye .Fundus examination revealed severe vitritis in the RE with retinitis lesions and hemorrhages and macular star ,Fundus examination of the left eye revealed moderate vitritis with retinitis lesions with hemorrhages and macular star. She was started on tab doxycycline 100 mg BD for 2 weeks and oral steroids. She was also advised RE intravitreal implant Ozurdex with explained prognosis.
Photographer: DR. TEJASWITA VERMA
Imaging device: MIRANTE
Condition/keywords: bilateral dengue retinitis, Dengue Fever, POST FEVER RETINITIS
-
 Post Dengue Fever Retinitis
Post Dengue Fever Retinitis
Dec 27 2024 by Tejaswita Verma
A 35 year old female presented with bilaterally decreased vision since a month post dengue fever. Vision was finger counting 6 mt. in the RE and 6/36 in the left eye .Fundus examination revealed severe vitritis in the RE with retinitis lesions and hemorrhages and macular star ,Fundus examination of the left eye revealed moderate vitritis with retinitis lesions with hemorrhages and macular star. She was started on tab doxycycline 100 mg BD for 2 weeks and oral steroids
Photographer: DR. TEJASWITA VERMA
Imaging device: MIRANTE
Condition/keywords: Dengue Fever, macular star, POST FEVER RETINITIS
-
 Toxoplasmosis
Toxoplasmosis
Dec 5 2024 by Tejaswita Verma
26 year old male with 6/18 vision , anterior chamber reaction, vitritis and retinitis lesion along the superotemporal arcade with full thickness involvement on OCT . FFA showing hypofluorescence with surrounding hyperfluorescence characterstic of toxoplasma retinitis . ICGA shows hypocyanescence.
Photographer: DR. TEJASWITA VERMA
Imaging device: MIRANTE
Condition/keywords: Fundus Fluorescein Angiography, indocyanine green (ICG) angiography, toxoplasmosis
-
 Uveal Effusion Syndrome
Uveal Effusion Syndrome
Sep 19 2024 by Virginia Gebhart
61 year old female with idiopathic uveal effusion syndrome. 360 degrees of choroidal thickening, especially anterior with exudative fluid inferior. Mild vitritis present. Unable to gain venous access for FA, ultrasound and UBM performed which confirm choroidal and ciliary body thickening. Pt sent for inflammatory work up including MRI of brain and orbits. Treatment pending results.
Photographer: Virginia Gebhart, Retina Consultants of Carolina
Imaging device: Optos California
Condition/keywords: idiopathic uveal effusion syndrome, uveal effusion
-
 Atypical Tubercular Peripheral Occlusive Retinal Vasculitis
Atypical Tubercular Peripheral Occlusive Retinal Vasculitis
Jun 21 2024 by Tejaswita Verma
Fundus montage of the right eye of a 27 year old male with macula threatening occlusive vasculitis showing hemorrhages in inferior, temporal quadrant with vascular sheathing. The patient was Mantoux positive (20 mm induration) and IGRA (TB-GOLD)positive and started on oral steroids. The case was atypical due to no vitritis at presentation which is unusual of tuberculosis. Behcet's disease was ruled out as there was no panuveitis like picture.
Photographer: DR. TEJASWITA VERMA
Imaging device: MIRANTE
Condition/keywords: occlusive vasculitis, ocular tuberculosis
-
Toxoplasmosis Chorioretinitis
Mar 2 2024 by James P Dossett, MD
Pseudocolor fundus photograph of the right eye of a 34-year-old man with retinitis along the inferotemporal arcade with associated subretinal fluid and overlying vitritis. Aqueous paracentesis was performed and PCR was positive for Toxoplasma gondii. He was administered intravitreal clindamycin.
Imaging device: Optos
Condition/keywords: posterior uveitis, toxoplasmosis chorioretinitis
-
 CMV Retinitis with Shallow RD
CMV Retinitis with Shallow RD
Aug 21 2023 by rahul saradge
47 YEAR OLD MALE HAVING CMV RETINITIS WITH SHALLOW RD, VITRITIS
Photographer: Hitesh Rawlani , Isha Netralaya
Condition/keywords: cmv retinits with shallow RD
-
 Chorioretinitis with Overlying Vitreous Stranding/Vitritis
Chorioretinitis with Overlying Vitreous Stranding/Vitritis
Mar 23 2023 by Isaac Agranoff
Fundus photograph of a 37-year-old woman presenting with chorioretinitis with overlying vitreous stranding/vitritis that has remained unchanged for multiple years. Patient presented with irritation and blurred vision and her vision was 20/40 OD. The OCT revealed evidence of low-grade inflammation and the recommend treatment was anti-inflammatory eye drops at this time and to obtain second opinion with another physician in the office.
Photographer: Isaac Agranoff, Technician
Imaging device: Optos California
Condition/keywords: chorioretinal scar, chorioretinitis, inflammation, Optos, ultra-wide field imaging, vitritis
-
 acute posterior multifocal placoid pigment epitheliopathy
acute posterior multifocal placoid pigment epitheliopathy
Sep 23 2022 by Jaideep sharma
A 50-year old woman presented to us with unilateral progressive and painless visual blurring. She was diagnosed as a case of CSCR and started on topical dorzolamide with no improvement in VA. Her best-corrected visual acuity (BCVA) was RE 6/6 and LE 6/60 . Eye examination revealed vitritis (grade1) with optic disc hyperemia and multiple serous retinal detachments with choroidal striae in the left eye and a normal right eye. She is k/c/o diabetes. Her past ocular and drug histories were unremarkable. Retinal imaging revealed characteristic features of APMPPE in the left eye. All laboratory testing results were inconclusive. VA and OCT findings significantly improved following the treatment with LE posterior sub tenon’s triamcinolone (40 mg/ml). 1 month post injection VA of the left eye reached 6/6 with resolved serous retinal detachments in this eye. This case is unique as it was managed via PST injection rather than conventional steroid therapy
Photographer: jaideep sharma jaipur calgary eye hospital rajasthan india
Condition/keywords: acute posterior multifocal placoid pigment epitheliopathy (APMPPE), FFA
-
 Acute posterior multifocal placoid pigment epitheliopathy (APMPPE)
Acute posterior multifocal placoid pigment epitheliopathy (APMPPE)
Sep 23 2022 by Jaideep sharma
A 50-year old woman presented to us with unilateral progressive and painless visual blurring. She was diagnosed as a case of CSCR and started on topical dorzolamide with no improvement in VA. Her best-corrected visual acuity (BCVA) was RE 6/6 and LE 6/60 . Eye examination revealed vitritis (grade1) with optic disc hyperemia and multiple serous retinal detachments with choroidal striae in the left eye and a normal right eye. She is k/c/o diabetes. Her past ocular and drug histories were unremarkable. Retinal imaging revealed characteristic features of APMPPE in the left eye. All laboratory testing results were inconclusive. VA and OCT findings significantly improved following the treatment with LE posterior sub tenon’s triamcinolone (40 mg/ml). 1 month post injection VA of the left eye reached 6/6 with resolved serous retinal detachments in this eye. This case is unique as it was managed via PST injection rather than conventional steroid therapy
Photographer: jaideep sharma jaipur calgary eye hospital rajasthan india
Condition/keywords: acute posterior multifocal placoid pigment epitheliopathy (APMPPE), FFA
-
 Recurrence of Ocular Toxoplasmosis
Recurrence of Ocular Toxoplasmosis
Apr 11 2022 by Aniruddha K Agarwal, MD
Inactive toxoplasmosis lesion with active lesion at the inferior edge. The active lesion appears "fuzzy". Note also the overlying vitritis
Photographer: Debra A. Goldstein, MD, FRCSC Magerstadt Professor of Ophthalmology Director, Uveitis Service Director, Uveitis Fellowship Department of Ophthalmology Northwestern University Feinberg School of Medicine
Condition/keywords: IUSG, recurrence, retinochoroiditis, toxoplasmosis chorioretinitis, uveitis
-
 Fundus Photo Montage showing Occlusive Vascultis from Brolucizumab
Fundus Photo Montage showing Occlusive Vascultis from Brolucizumab
Jan 21 2022 by Somnath Chakraborty, MD
Right eye of a 62-year-old lady with Inferotemporal Branch Retinal Vein Occlusion, treated with single dose of "off-label" brolucizumab. She developed Occlusive Vasculitis 9 weeks post injection. This is her Fundus Photo Montage at that time, showing evidence of Occlusive Vasculitis with moderate grade vitritis. BCVA OD 20/400.
Photographer: Pulak Roy
Condition/keywords: branch retinal vein occlusion (BRVO), Brolucizumab, occlusive vasculitis, vitritis
-
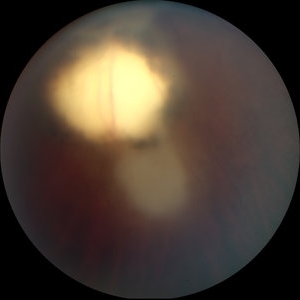
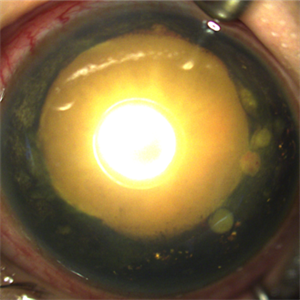
 Necrotic Multifocal Retinoblastoma Group E (ICRB) / cT3e (AJCC)
Necrotic Multifocal Retinoblastoma Group E (ICRB) / cT3e (AJCC)
Jul 7 2021 by Linda A Cernichiaro- Espinosa, MD
A 3-year, 9-month-old male presented with unilateral advanced group E multifocal retinoblastoma cT3e (AJCC). Anterior seeding vascularized over the iris surface. Fluorescein angiogram fills the vascularized tumors. Aseptic orbital cellulitis, birefringent anterior segment crystals, cataract and dense vitritis are secondary to necrosis.
Photographer: Jose Oyervides-Alvarado MD
Imaging device: RetCam3
Condition/keywords: fluorescein angiogram (FA), pediatric tumor, retinoblastoma
-
 Necrotic Multifocal Retinoblastoma Group E (ICRB) / cT3e (AJCC)
Necrotic Multifocal Retinoblastoma Group E (ICRB) / cT3e (AJCC)
Jul 7 2021 by Linda A Cernichiaro- Espinosa, MD
A 3-year, 9-month-old male presented with unilateral advanced group E multifocal retinoblastoma cT3e (AJCC). Anterior seeding vascularized over the iris surface. Fluorescein angiogram fills the vascularized tumors. Aseptic orbital cellulitis, birefringent anterior segment crystals, cataract and dense vitritis are secondary to necrosis.
Photographer: Jose Oyervides-Alvarado MD
Imaging device: RetCam3
Condition/keywords: retinoblastoma
-
 Toxoplasmic Retinitis
Toxoplasmic Retinitis
Feb 11 2021 by David L Kilpatrick, MD
A 50-year-old female presented with a history of subacute central vision loss involving the right eye. Exam showed a focal, creamy white retinitis involving the fovea with mild vitritis. FA demonstrates blockage of the lesion initially followed by progressive leakage, most prominently at the border of the retinitis. Toxoplasma IgM and IgG were both markedly elevated. The patient was treated with a combination of Bactrim, Intravitreal Clindamycin, and Oral steroids.
Photographer: MS Retina Associoates
Imaging device: Optos
Condition/keywords: toxoplasmosis chorioretinitis, toxoplasmosis retinitis
-
 Palms of Patient with Placoid Lesions in Posterior Segment
Palms of Patient with Placoid Lesions in Posterior Segment
Dec 20 2020 by John S. King, MD
44-year-old white female seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), Plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU. Va 20/200 OD and 20/20 OS, IOP 12 OU, Pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery. There was trace vitreous cell OS, mild disc edema, and a large, granular placoid area nasally that appeared to be granulated. The OCT showed mild subfoveal fluid with nodular areas in the RPE and some overlying irregular architecture of the outer retina. Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand (See Image), and later learned that she had a rash on the soles of her feet. She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started). She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated. OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer.
Imaging device: Optos CA
Condition/keywords: acute syphilitic posterior placoid chorioretinitis
-
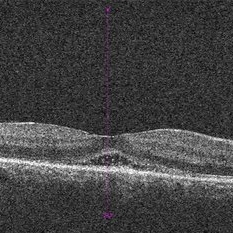 Posterior Placoid Chorioretinopathy
Posterior Placoid Chorioretinopathy
Dec 19 2020 by John S. King, MD
44-year-old white female seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU. Va 20/200 OD and 20/20 OS, IOP 12 OU, pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery. There was a trace vitreous cell OS with a large, granular placoid lesion nasally. The OCT (see above) shows mild subfoveal fluid with nodular areas in the RPE and some overlying irregular architecture of the outer retina. Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand, and later learned that she had a rash on the soles of her feet. She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started). She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated. OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer.
Imaging device: Zeiss Cirrus
Condition/keywords: acute syphilitic posterior placoid chorioretinitis, syphilis
-
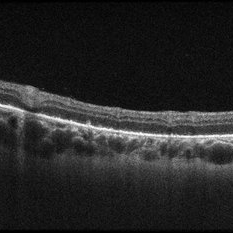 Posterior Placoid Chorioretinopathy
Posterior Placoid Chorioretinopathy
Dec 19 2020 by John S. King, MD
44-year-old white female seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU. Va 20/200 OD and 20/20 OS, IOP 12 OU, pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery. There was a trace vitreous cell OS with a large, granular placoid lesion nasally. The OCT via the lesion (see above) shows nodular areas in the RPE and some overlying disruption of EZ and outer retina. Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand, and later learned that she had a rash on the soles of her feet. She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started). She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated. OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer.
Imaging device: Zeiss Cirrus
Condition/keywords: acute syphilitic posterior placoid chorioretinitis, syphilis
-
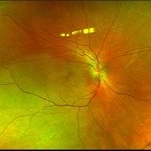 Posterior Placoid Chorioretinopathy
Posterior Placoid Chorioretinopathy
Dec 19 2020 by John S. King, MD
44-year-old white female seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU. Va 20/200 OD and 20/20 OS, IOP 12 OU, pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery. There was trace vitreous cell OS, mild disc edema, and a large, granular placoid area nasally that appeared to be granulated. The OCT showed mild subfoveal fluid with nodular areas in the RPE and some overlying irregular architecture of the outer retina. Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand, and later learned that she had a rash on the soles of her feet. She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started). She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated (See Image). OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer.
Photographer: Ashley Seiger
Imaging device: Optos CA
Condition/keywords: acute syphilitic posterior placoid chorioretinitis

 Loading…
Loading…