Search results (64 results)
-
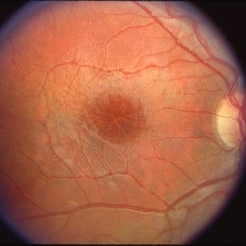
 Best Vitelliform Macular Dystrophy
Best Vitelliform Macular Dystrophy
Dec 24 2025 by KANWALJEET HARJOT MADAN, M.S. (Ophthalmology); FAICO (Vitreous - Retina)
This is Fundus Autofluorescence (FAF) image of LE of a 7 year-old boy. He was diagnosed to have retinal lesions in BE elsewhere. Fundus exam revealed presence of egg yolk macular lesions in BE which depicted intense hyper autofluorescence. He was diagnosed to have Best Vitelliform Macular Dystrophy. It is an autosomal dominant condition caused by mutations in BEST 1 Gene and leads to accumulation of lipofuscin in subretinal space.
Photographer: Dr. Kanwaljeet Harjot Madan, Thind Eye Hospital, Jalandhar City (Punjab) INDIA.
Imaging device: Zeiss Fundus Camera
Condition/keywords: Best vitelliform macular dystrophy (BVMD)
-
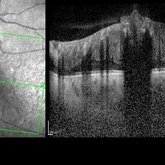
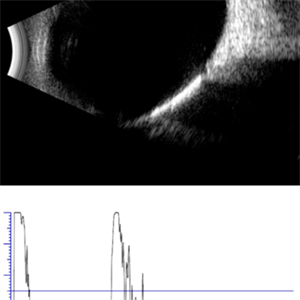 Choroidal Osteoma
Choroidal Osteoma
Apr 17 2025 by Gustavo Uriel Fonseca Aguirre
Top (B-mode): The longitudinal scan reveals a hyperechoic, flat, and well-demarcated macular lesion with posterior acoustic shadowing, pathognomonic for choroidal osteoma. Bottom (A-mode): Standardized tracing shows a tall initial spike (100% reflectivity) at the tumor surface with rapid decay to acoustic silence, confirming sound absorption by calcified tissue. This pattern remains unchanged at variable gain settings.
Photographer: Gustavo U. Fonseca Aguirre, Hospital Conde de Valenciana, Ciudad de México
Condition/keywords: choroidal osteoma, macular choroidal osteoma
-
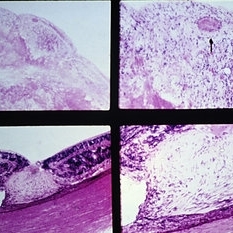
 Best Vitelliform Macular Dystrophy
Best Vitelliform Macular Dystrophy
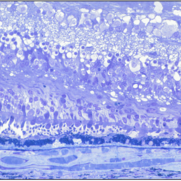
Dec 10 2020 by McGill University Health Centre
Postmortem eyes from 101-year-old female. Past clinical history includes a poor vision for many years due to macular degeneration. The last visual acuity test recorded 6/15 OD and 6/6 OS. IOP 14 and 18 torr OS. Histopathology: Disclosed and yellow 2x2mm macular lesion. Microscopic examination: elevated placoid macular lesion with overlying pigment granules. Electron microscopy examination: pigment granules with abundant lipofuscin and melanolysosomes, photoreceptor cells markedly attenuated (less degenerated at the periphery) Numerous calcified drusen throughout the retina particularly in the posterior pole. RPE lipofuscin content is elevated in Best’s dystrophy. The extractability of the PRE lipofuscin fluorophores is reduced (it is normal during senescence). The defect in Best’s dystrophy accelerates this age related change in lipofuscin.
Condition/keywords: Best vitelliform macular dystrophy (BVMD), histopathology, pathology
-
 Best Vitelliform Macular Dystrophy
Best Vitelliform Macular Dystrophy
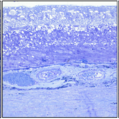
Dec 10 2020 by McGill University Health Centre
Postmortem eyes from 101-year-old female. Past clinical history includes a poor vision for many years due to macular degeneration. The last visual acuity test recorded 6/15 OD and 6/6 OS. IOP 14 and 18 torr OS. Histopathology: Disclosed and yellow 2x2mm macular lesion. Microscopic examination: elevated placoid macular lesion with overlying pigment granules. Electron microscopy examination: pigment granules with abundant lipofuscin and melanolysosomes, photoreceptor cells markedly attenuated (less degenerated at the periphery) Numerous calcified drusen throughout the retina particularly in the posterior pole. RPE lipofuscin content is elevated in Best’s dystrophy. The extractability of the PRE lipofuscin fluorophores is reduced (it is normal during senescence). The defect in Best’s dystrophy accelerates this age related change in lipofuscin.
Condition/keywords: Best vitelliform macular dystrophy (BVMD), histopathology, pathology
-
 Best Vitelliform Macular Dystrophy
Best Vitelliform Macular Dystrophy
Dec 10 2020 by McGill University Health Centre
Postmortem eyes from 101-year-old female. Past clinical history includes a poor vision for many years due to macular degeneration. The last Visual acuity test recorded 6/15 OD and 6/6 OS. IOP 14 and 18 torr OS. Histopathology: Disclosed and yellow 2x2mm macular lesion. Microscopic examination: elevated placoid macular lesion with overlying pigment granules. Electron microscopy examination: pigment granules with abundant lipofuscin and melanolysosomes, photoreceptor cells markedly attenuated (less degenerated at the periphery) Numerous calcified drusen throughout the retina particularly in the posterior pole. RPE lipofuscin content is elevated in Best’s dystrophy. The extractability of the PRE lipofuscin fluorophores is reduced (it is normal during senescence). The defect in Best’s dystrophy accelerates this age related change in lipofuscin.
Condition/keywords: Best vitelliform macular dystrophy (BVMD), histopathology, pathology
-
 Best Vitelliform Macular Dystrophy
Best Vitelliform Macular Dystrophy
Dec 10 2020 by McGill University Health Centre
Postmortem eyes from 101-year-old female. Past clinical history includes a poor vision for many years due to macular degeneration. The last visual acuity test recorded 6/15 OD and 6/6 OS. IOP 14 and 18 torr OS. Histopathology: Disclosed and yellow 2x2mm macular lesion. Microscopic examination: elevated placoid macular lesion with overlying pigment granules. Electron microscopy examination: pigment granules with abundant lipofuscin and melanolysosomes, photoreceptor cells markedly attenuated (less degenerated at the periphery) Numerous calcified drusen throughout the retina particularly in the posterior pole. RPE lipofuscin content is elevated in Best’s dystrophy. The extractability of the PRE lipofuscin fluorophores is reduced (it is normal during senescence). The defect in Best’s dystrophy accelerates this age related change in lipofuscin.
Condition/keywords: Best vitelliform macular dystrophy (BVMD), fundus photograph
-
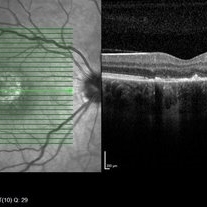
 Combined Hamartoma of the Retina and Retinal Pigment Epithelium (CHRRPE)
Combined Hamartoma of the Retina and Retinal Pigment Epithelium (CHRRPE)
Jan 21 2020 by Pierre-Henry Gabrielle, MD
Coupled OCT B-scan and IR imaging of a 17-year-old man with combined hamartomas of the retina and retinal pigment epithelium (CHRRPE) at the posterior pole of the left eye. One can see a highly reflective elevated macular lesion with hyporeflective shadowing of the underlying tissue and obscuration of the normal retinal layers.
Photographer: Pierre-Henry Gabrielle, Ophthalmology department, Dijon University Hospital, France
Imaging device: Heidelberg Spectralis
Condition/keywords: combined hamartoma, optical coherence tomography (OCT)
-
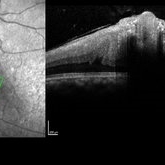
 Combined Hamartoma of the Retina and Retinal Pigment Epithelium (CHRRPE)
Combined Hamartoma of the Retina and Retinal Pigment Epithelium (CHRRPE)
Jan 21 2020 by Pierre-Henry Gabrielle, MD
Coupled OCT B-scan and IR imaging of a 17-year-old man with Combined hamartomas of the retina and retinal pigment epithelium (CHRRPE) at the posterior pole of the left eye. One can see a highly reflective elevated macular lesion with hyporeflective shadowing of the underlying tissue and obscuration of the normal retinal layers.
Photographer: Pierre-Henry Gabrielle, Ophthalmology department, Dijon University Hospital, France
Imaging device: Heidelberg Spectralis
Condition/keywords: combined hamartoma, optical coherence tomography (OCT)
-
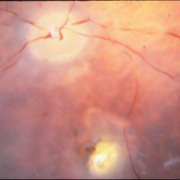
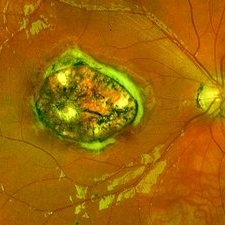 Congenital Toxoplasmosis
Congenital Toxoplasmosis
Dec 18 2019 by Yoshihiro Yonekawa, MD, FASRS
Widefield fundus image of a teenage girl's right eye with an inactive congenital toxoplasmosis macular lesion. Her vision is 20/400 in this eye.
Photographer: Netanya Lerner, COA, Wills Eye Hospital/Mid Atlantic Retina
Imaging device: Optos California
Condition/keywords: congenital toxoplasmosis, pediatric retina
-
Unilateral Acute Idiopathic Maculopathy FA
May 7 2019 by William Ensor
A 37-year-old female presented with a two-week history of vision loss in the right eye. She experienced a flu-like illness including rash on the hands, feet, and mouth 2 days prior to her vision change. Her 3-year-old son had a similar illness diagnosed as hand, foot, and mouth disease by his pediatrician one week prior. Her visual acuity was 20/150 of the right eye, and 20/20 of the left eye. On dilated fundus examination, the left eye was unremarkable; the right eye revealed a circular, variably pigmented lesion of the macula. OCT imaging showed areas of RPE loss and clumping, with overlying loss of the photoreceptor layer. Fluorescein angiography showed central and peripheral hyperfluorescence consistent with window defect, and blockage in area of RPE loss. No treatment was initiated at this time. The patient returned 10 days later; her visual acuity improved to 20/50 in the right eye. Dilated fundus exam showed increased pigmentation of the macular lesion. OCT of the right eye showed further RPE clumping without recovery of the photoreceptor layer, despite her improved visual acuity.
Condition/keywords: unilateral acute idiopathic maculopathy
-
Unilateral Acute Idiopathic Maculopathy FA
May 7 2019 by William Ensor
A 37-year-old female presented with a two-week history of vision loss in the right eye. She experienced a flu-like illness including rash on the hands, feet, and mouth 2 days prior to her vision change. Her 3-year-old son had a similar illness diagnosed as hand, foot, and mouth disease by his pediatrician one week prior. Her visual acuity was 20/150 of the right eye, and 20/20 of the left eye. On dilated fundus examination, the left eye was unremarkable; the right eye revealed a circular, variably pigmented lesion of the macula. OCT imaging showed areas of RPE loss and clumping, with overlying loss of the photoreceptor layer. Fluorescein angiography showed central and peripheral hyperfluorescence consistent with window defect, and blockage in area of RPE loss. No treatment was initiated at this time. The patient returned 10 days later; her visual acuity improved to 20/50 in the right eye. Dilated fundus exam showed increased pigmentation of the macular lesion. OCT of the right eye showed further RPE clumping without recovery of the photoreceptor layer, despite her improved visual acuity.
Condition/keywords: unilateral acute idiopathic maculopathy
-
Unilateral Acute Idiopathic Maculopathy Fundus
May 7 2019 by William Ensor
A 37-year-old female presented with a two-week history of vision loss in the right eye. She experienced a flu-like illness including rash on the hands, feet, and mouth 2 days prior to her vision change. Her 3-year-old son had a similar illness diagnosed as hand, foot, and mouth disease by his pediatrician one week prior. Her visual acuity was 20/150 of the right eye, and 20/20 of the left eye. On dilated fundus examination, the left eye was unremarkable; the right eye revealed a circular, variably pigmented lesion of the macula. OCT imaging showed areas of RPE loss and clumping, with overlying loss of the photoreceptor layer. Fluorescein angiography showed central and peripheral hyperfluorescence consistent with window defect, and blockage in area of RPE loss. No treatment was initiated at this time. The patient returned 10 days later; her visual acuity improved to 20/50 in the right eye. Dilated fundus exam showed increased pigmentation of the macular lesion. OCT of the right eye showed further RPE clumping without recovery of the photoreceptor layer, despite her improved visual acuity.
Condition/keywords: unilateral acute idiopathic maculopathy
-
Unilateral Acute Idiopathic Maculopathy Fundus
May 7 2019 by William Ensor
A 37-year-old female presented with a two-week history of vision loss in the right eye. She experienced a flu-like illness including rash on the hands, feet, and mouth 2 days prior to her vision change. Her 3-year-old son had a similar illness diagnosed as hand, foot, and mouth disease by his pediatrician one week prior. Her visual acuity was 20/150 of the right eye, and 20/20 of the left eye. On dilated fundus examination, the left eye was unremarkable; the right eye revealed a circular, variably pigmented lesion of the macula. OCT imaging showed areas of RPE loss and clumping, with overlying loss of the photoreceptor layer. Fluorescein angiography showed central and peripheral hyperfluorescence consistent with window defect, and blockage in area of RPE loss. No treatment was initiated at this time. The patient returned 10 days later; her visual acuity improved to 20/50 in the right eye. Dilated fundus exam showed increased pigmentation of the macular lesion. OCT of the right eye showed further RPE clumping without recovery of the photoreceptor layer, despite her improved visual acuity.
Condition/keywords: unilateral acute idiopathic maculopathy
-
Unilateral Acute Idiopathic Maculopathy Fundus
May 7 2019 by William Ensor
A 37-year-old female presented with a two-week history of vision loss in the right eye. She experienced a flu-like illness including rash on the hands, feet, and mouth 2 days prior to her vision change. Her 3-year-old son had a similar illness diagnosed as hand, foot, and mouth disease by his pediatrician one week prior. Her visual acuity was 20/150 of the right eye, and 20/20 of the left eye. On dilated fundus examination, the left eye was unremarkable; the right eye revealed a circular, variably pigmented lesion of the macula. OCT imaging showed areas of RPE loss and clumping, with overlying loss of the photoreceptor layer. Fluorescein angiography showed central and peripheral hyperfluorescence consistent with window defect, and blockage in area of RPE loss. No treatment was initiated at this time. The patient returned 10 days later; her visual acuity improved to 20/50 in the right eye. Dilated fundus exam showed increased pigmentation of the macular lesion. OCT of the right eye showed further RPE clumping without recovery of the photoreceptor layer, despite her improved visual acuity.
Condition/keywords: unilateral acute idiopathic maculopathy
-
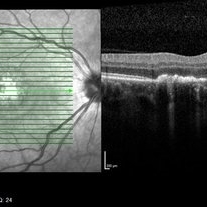 Unilateral Acute Idiopathic Maculopathy OCT Macula
Unilateral Acute Idiopathic Maculopathy OCT Macula
May 7 2019 by William Ensor
A 37-year-old female presented with a two-week history of vision loss in the right eye. She experienced a flu-like illness including rash on the hands, feet, and mouth 2 days prior to her vision change. Her 3-year-old son had a similar illness diagnosed as hand, foot, and mouth disease by his pediatrician one week prior. Her visual acuity was 20/150 of the right eye, and 20/20 of the left eye. On dilated fundus examination, the left eye was unremarkable; the right eye revealed a circular, variably pigmented lesion of the macula. OCT imaging showed areas of RPE loss and clumping, with overlying loss of the photoreceptor layer. Fluorescein angiography showed central and peripheral hyperfluorescence consistent with window defect, and blockage in area of RPE loss. No treatment was initiated at this time. The patient returned 10 days later; her visual acuity improved to 20/50 in the right eye. Dilated fundus exam showed increased pigmentation of the macular lesion. OCT of the right eye showed further RPE clumping without recovery of the photoreceptor layer, despite her improved visual acuity.
Condition/keywords: unilateral acute idiopathic maculopathy
-
 Unilateral Acute Idiopathic Maculopathy OCT Macula
Unilateral Acute Idiopathic Maculopathy OCT Macula
May 7 2019 by William Ensor
A 37-year-old female presented with a two-week history of vision loss in the right eye. She experienced a flu-like illness including rash on the hands, feet, and mouth 2 days prior to her vision change. Her 3-year-old son had a similar illness diagnosed as hand, foot, and mouth disease by his pediatrician one week prior. Her visual acuity was 20/150 of the right eye, and 20/20 of the left eye. On dilated fundus examination, the left eye was unremarkable; the right eye revealed a circular, variably pigmented lesion of the macula. OCT imaging showed areas of RPE loss and clumping, with overlying loss of the photoreceptor layer. Fluorescein angiography showed central and peripheral hyperfluorescence consistent with window defect, and blockage in area of RPE loss. No treatment was initiated at this time. The patient returned 10 days later; her visual acuity improved to 20/50 in the right eye. Dilated fundus exam showed increased pigmentation of the macular lesion. OCT of the right eye showed further RPE clumping without recovery of the photoreceptor layer, despite her improved visual acuity.
Condition/keywords: unilateral acute idiopathic maculopathy
-
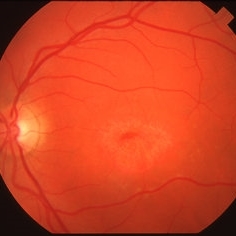
 Congenital Toxoplasmosis
Congenital Toxoplasmosis
Apr 8 2019 by Gary R. Cook, MD, FACS
Right eye of a 23-year-old male with congenital toxoplasmosis OD; view of macular lesion.
Condition/keywords: congenital toxoplasmosis, inactive toxoplasmosis, macular scar, ocular toxoplasmosis
-
 Stargardt's Disease
Stargardt's Disease
Apr 8 2019 by Gary R. Cook, MD, FACS
38-year-old white male with atrophic macular lesion OS secondary to Stargardt's disease; V.A. = 20/200
Imaging device: Topcon VT-50
Condition/keywords: atrophic central lesion, Stargardt disease
-
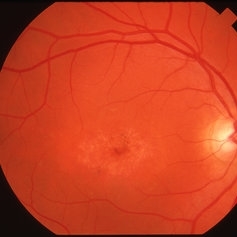 Stargardt's Disease
Stargardt's Disease
Apr 8 2019 by Gary R. Cook, MD, FACS
38-year-old white male with typical atrophic macular lesion OD secondary to Stargardt's disease; V.A. = 20/200
Imaging device: Topcon VT-50
Condition/keywords: atrophic central lesion, Stargardt disease
-
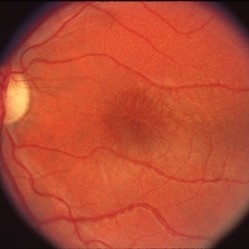 Stellate Maculopathy in Juvenile Retinoschisis
Stellate Maculopathy in Juvenile Retinoschisis
Apr 2 2019 by Gary R. Cook, MD, FACS
10-year old white male with stellate macular lesion OS due to juvenile retinoschisis.
Condition/keywords: juvenile retinoschisis, retinoschisis, stellate maculopathy
-
 Juvenile Retinoschisis
Juvenile Retinoschisis
Apr 2 2019 by Gary R. Cook, MD, FACS
10-year old white male with stellate macular lesion OD secondary to juvenile retinoschisis; V.A. = 20/100
Condition/keywords: juvenile retinoschisis, retinoschisis, stellate maculopathy
-
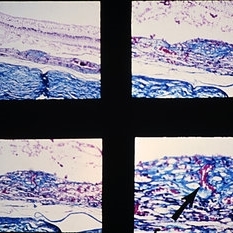
 Slide 9-98
Slide 9-98
Feb 26 2019 by Lancaster Course in Ophthalmology
Coats' disease with disciform macular lesion. There is accumulation of periodic acid-Schiff-positive staining material within and under the retina peripherally (upper left), in association with telangiectatic retinal vessels (arrow , upper right) . A fibrous nodule is present under the retina in the macular area (lower views). The laminated appearance and partial pigmentation suggest that this fibrous nodule is in part derived from hyperplastic retinal pigment epithelium (lower right).
Condition/keywords: Coats' disease, disciform macular lesion
-
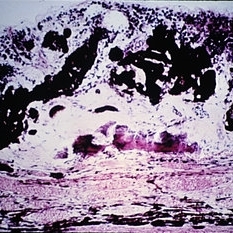 Slide 9-97
Slide 9-97
Feb 26 2019 by Lancaster Course in Ophthalmology
Disciform macular lesion with marked hyperplasia of RPE (A.F.I.P. No. 797119).
Condition/keywords: disciform macular lesion, hyperplasia, retinal pigment epithelium
-
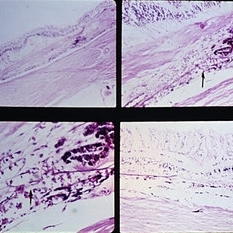 Slide 9-95
Slide 9-95
Feb 26 2019 by Lancaster Course in Ophthalmology
Macular disciform lesion in a 73-year-old man with angioid streaks and pseudoxanthoma elasticum. The streak is subjacent to the scar and is the point at which choroidal vessels (arrows) extend internally. The same streak closer to the disc is shown in the lower right view.
Condition/keywords: angioid streaks, disciform macular lesion, pseudoxanthoma elasticum (PXE)
-
 Slide 9-94
Slide 9-94
Feb 26 2019 by Lancaster Course in Ophthalmology
Macular disciform lesion in the ocular histoplasmosis syndrome. Note choroidal scar with vessels (arrow) extending through a break in Bruch's membrane.
Condition/keywords: Bruch's membrane, disciform macular lesion, ocular histoplasmosis syndrome (OHS)

 Loading…
Loading…