-
 By Rinal Pandit
By Rinal Pandit
Dr. - Uploaded on Sep 2, 2020.
- Last modified by Rinal Pandit on Sep 3, 2020.
- Rating
- Appears in
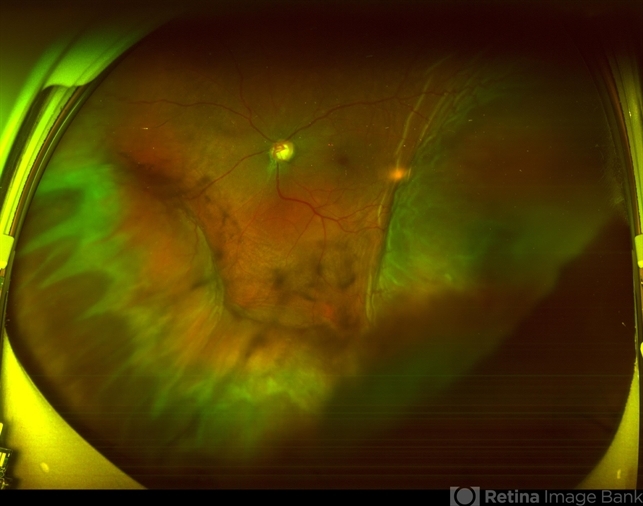
- FUNDUS PHOTO
- Condition/keywords
- trabeculectomy, suprachoroidal hemorrhage, ultra-wide field imaging
- Imaging device
-
Fundus camera
OPTOS,Ultra wide field retinal imaging system - Description
- Fundus photograph of left eye of a 56-year-old female with primary angle closure glaucoma showing massive hemorrhagic choroidal detachment that developed following trabeculectomy surgery. Suprachoroidal hemorrhage is defined as the accumulation of blood within the potential space between the choroid and sclera, with the source of the blood being the long or short posterior ciliary artery. Delayed suprachoroidal hemorrhage (DSHC) remains one of the most dreaded and sight threatening complications of glaucoma filtration surgery. The risk factors include old age, hypertension, high myopia, arteriosclerosis, chronically elevated IOP, sudden hypotony, trauma, aphakia/pseudophakia, prior vitrectomy, history of 5 FU injections and anti-platelet agents. The incidence of postoperative SCH after trabeculectomy varies between 0.6%- 1.4%. DSCH after surgery varies considerably in severity but is generally characterized by the sudden onset of severe pain, decreased vision, and a shallow anterior chamber usually associated with raised intraocular pressure. B-scan ultrasonography can help to distinguish serous from hemorrhagic choroidals.Suprachoroidal hemorrhages appear as dome-shaped elevations of the retina with increased echo densities that are often heterogeneous and within the suprachoroidal space. Choroidal effusions appear as dome-shaped elevations with hypoechoic suprachoroidal space. The first step in the management is the timely diagnosis. Medical management includes oral and topical antiglaucoma drugs to lower IOP, oral and topical steroids to control inflammation and topical cycloplegics and oral analgesics to tackle pain. Serial ultrasound B scans of the affected eye should be performed in order to monitor progression of the SCH and help determine apposition, height, and liquefaction of the SCH. Indications of surgical drainage include non resolution with medical management,concurrent retinal detachment, central retinal apposition (kissing choroidals) and incarceration of vitreous in the wound site. The ideal time of drainage is between 7-14 days depending upon clot lysis. The prognosis of both intraoperative and postoperative SCH is poor. An overwhelming majority of patients do not achieve pre-hemorrhage visual acuity and most do not recover to a visual acuity of 20/200 or better. The major determinants of good or bad visual outcomes of SCH’s are preoperative visual acuity and retinal detachment at the time of hemorrhage, respectively.

 Initializing download.
Initializing download.






