Search results (13 results)
-
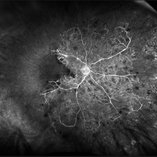
 Central Retinal Vein Occlusion With Macular Edema and Venous Beading
Central Retinal Vein Occlusion With Macular Edema and Venous Beading
Jun 18 2025 by Korey Starkey
64-year-old patient presents with CRVO with secondary macular edema in both eyes. Venous beading present in 2/4 quadrants OU. Patient also presents with severe non-proliferative diabetic retinopathy. Treatment recommended of anti-vegF intravitreal injections OU.
Photographer: Korey Starkey
Imaging device: Optos
Condition/keywords: attenuated vessels, central retinal vein occlusion (CRVO), CRVO, FA early phase, FLUORESCEIN ANGIOGRAPHY, macular edema, Optomap, OPTOS CALIFORNIA, severe NPDR, venous beading
-
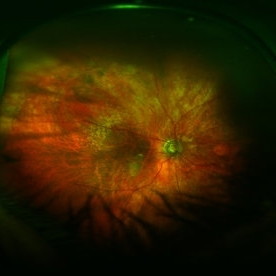
 Ischemic Central Retinal Vein Occlusion
Ischemic Central Retinal Vein Occlusion
Jan 24 2019 by Nichole Lewis
76-year-old woman with an ischemic central retinal vein occlusion, severely attenuated and sclerotic vessels and scattered retinal hemorrhages. Vision decrease over 1 year. VA 20/CF. Patient is returning for pan retinal photocoagulation.
Photographer: Nichole Lewis
Imaging device: Optos
Condition/keywords: attenuated vessels, central retinal vein occlusion (CRVO), hemorrhage, ischemic CRVO, sclerotic vessels
-
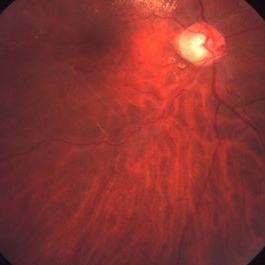
 Optic Atrophy and Attenuated Retinal Vessels Following Endophthalmitis
Optic Atrophy and Attenuated Retinal Vessels Following Endophthalmitis
Jul 12 2014 by Philip J. Polkinghorne, MD
This elderly lady underwent a vitrectomy for post-surgical endophthalmitis. The infection was successfully treated but the functional outcome was poor because of optic atrophy and attenuated retinal vessels.
Photographer: Alex Fraser
Imaging device: Optos Camera
Condition/keywords: attenuated vessels, endophthalmitis, optic atrophy, post-vitrectomy
-
 Regressed Proliferative Diabetic Retinopathy following PRP
Regressed Proliferative Diabetic Retinopathy following PRP
Sep 6 2012 by Sharon Fekrat, MD FACS FASRS
58-year-old man with regressed proliferative diabetic retinopathy in the left eye following panretinal laser photocoagulation. Note attenuated retinal vasculature.
Photographer: Sarah Enfiedjian, Ophthalmic Photographer, Durham VA Medical Center, Durham, NC
Imaging device: Zeiss
Condition/keywords: attenuated vessels, pan-retinal photocoagulation (PRP)
-
 CRAO Post COVID-19
CRAO Post COVID-19
May 21 2021 by Deepak Bhojwani, MS
Fundus Image of a 67-year old lady with history of COVID-19 disease 20 days back with elevated D-DIMER, CRP levels came to our clinic with sudden diminution of vision in her right eye since last 4 days. The fundus photo shows cherry red spot and severely attenuated vessels and pale disc suggesting classic CRAO. FFA was also done to confirm the same. We could only retrospectively attribute this artery occlusion secondary to recent past history of COVID disease since this lady had no other systemic co-morbidities.
Photographer: Deepak Bhojwani
Condition/keywords: central retinal artery occlusion (CRAO), COVID-19
-
 Ischemic BRVO
Ischemic BRVO
Aug 23 2012 by Gerardo Garcia-Aguirre, MD
Fundus photograph showing attenuated vessels in the inferotemporal area.
Photographer: Noemí Hernández, Asociación para Evitar la Ceguera en México
Condition/keywords: branch retinal vein occlusion (BRVO)
-
 Ischemic BRVO with Neovascularization
Ischemic BRVO with Neovascularization
Aug 23 2012 by Gerardo Garcia-Aguirre, MD
Fundus photograph showing attenuated vessels in the superotemporal quadrant.
Photographer: Noemí Hernández, Asociación para Evitar la Ceguera en México
Condition/keywords: branch retinal vein occlusion (BRVO), neovascularization (NV)
-
 Macular Colobomas in Congenital Zika Syndrome
Macular Colobomas in Congenital Zika Syndrome
Sep 26 2020 by Swati Agarwal-Sinha, MD, FASRS
Color fundus picture of the right (OD) and left (OS) eye of 3-day-old female infant with congenital Zika syndrome with bilateral macular colobomatous like chorioretinal atrophy, attenuated vessels, pigmentary changes, and optic disc pallor.
Photographer: Swati Agarwal-Sinha, MD
Condition/keywords: fundus photograph, macular coloboma, zika
-
 Moyamoya: FA 2 Min OD of an Acute CRAO with CRA Sparing
Moyamoya: FA 2 Min OD of an Acute CRAO with CRA Sparing
Nov 17 2019 by John S. King, MD
60-year-old white female presented with five days of acute vision loss in the right eye. She was seen initially by referring doctor after hours five days ago and diagnosed with a CRAO and sent to ED to be evaluated stroke team. Right ICA was 100% closed but completely bypassed. She called four days later c/o redness and eye pain; at this point prominent iris vessels were seen, and she was sent to us. Her background history includes a diagnosis of moyamoya (underwent bilateral cerebral artery bypass 2015); atorvastatin for hypercholesterolemia; ASA; no hx of HTN or heart disease. She had a scleral buckle repair OD in 2017 and later developed a thick ERM, which was repaired in 2018; on her previous visit her acuity was noted at 20/40. On presentation her visual acuity was HM OD and 20/15 OS. IOP was 8 OD and 10 OS. There were prominent iris vessels in the right eye, no cell or flare, and an IOL. The posterior segment exam showed diffuse retinal whitening with attenuated vessels and boxcarring; there was sparing retinal whitening in a central area of the macula that appeared to be supplied by a cilio-retina artery. The FA showed very slow filling of the retinal vessels; there was some early perfusion secondary to the cilio-retinal artery. At 7 minutes there was still significant areas of non-perfusion, as well as macular ischemia. Avastin was administered, and one week later, PRP was performed. On the day PRP was performed, the irregular iris vessels had regressed completely. She said that she had a "sliver" of vision centrally in that eye; her acuity was CF 2' and IOP 12.
Photographer: Gretchen Harper
Imaging device: Topcon
Condition/keywords: central retinal artery occlusion (CRAO), cilioretinal sparing, moyamoya, neovascularization of iris (NVI)
-
 Moyamoya: FA 3:25 OD of an Acute CRAO with CRA Sparing
Moyamoya: FA 3:25 OD of an Acute CRAO with CRA Sparing
Nov 17 2019 by John S. King, MD
60-year-old white female presented with five days of acute vision loss in the right eye. She was seen initially by referring doctor after hours five days ago and diagnosed with a CRAO and sent to ED to be evaluated stroke team. Right ICA was 100% closed but completely bypassed. She called four days later c/o redness and eye pain; at this point prominent iris vessels were seen, and she was sent to us. Her background history includes a diagnosis of Moyamoya (underwent bilateral cerebral artery bypass 2015); atorvastatin for hypercholesterolemia; ASA; no hx of HTN or heart disease. She had a scleral buckle repair OD in 2017 and later developed a thick ERM, which was repaired in 2018; on her previous visit her acuity was noted at 20/40. On presentation her visual acuity was HM OD and 20/15 OS. IOP was 8 OD and 10 OS. There were prominent iris vessels in the right eye, no cell or flare, and an IOL. The posterior segment exam showed diffuse retinal whitening with attenuated vessels and boxcarring; there was sparing retinal whitening in a central area of the macula that appeared to be supplied by a cilio-retina artery. The FA showed very slow filling of the retinal vessels; there was some early perfusion secondary to the cilio-retinal artery. At 7 minutes there was still significant areas of non-perfusion, as well as macular ischemia. Avastin was administered, and one week later, PRP was performed. On the day PRP was performed, the irregular iris vessels had regressed completely. She said that she had a "sliver" of vision centrally in that eye; her acuity was CF 2' and IOP 12.
Photographer: Gretchen Harper
Imaging device: Topcon
Condition/keywords: central retinal artery occlusion (CRAO), cilioretinal sparing, moyamoya, neovascularization of iris (NVI)
-
 Moyamoya: FA 52 Sec OD of an Acute CRAO with CRA Sparing
Moyamoya: FA 52 Sec OD of an Acute CRAO with CRA Sparing
Nov 17 2019 by John S. King, MD
60-year-old white female presented with five days of acute vision loss in the right eye. She was seen initially by referring doctor after hours five days ago and diagnosed with a CRAO and sent to ED to be evaluated stroke team. Right ICA was 100% closed but completely bypassed. She called four days later c/o redness and eye pain; at this point prominent iris vessels were seen, and she was sent to us. Her background history includes a diagnosis of moyamoya (underwent bilateral cerebral artery bypass 2015); atorvastatin for hypercholesterolemia; ASA; no hx of HTN or heart disease. She had a scleral buckle repair OD in 2017 and later developed a thick ERM, which was repaired in 2018; on her previous visit her acuity was noted at 20/40. On presentation her visual acuity was HM OD and 20/15 OS. IOP was 8 OD and 10 OS. There were prominent iris vessels in the right eye, no cell or flare, and an IOL. The posterior segment exam showed diffuse retinal whitening with attenuated vessels and boxcarring; there was sparing retinal whitening in a central area of the macula that appeared to be supplied by a cilio-retina artery. The FA showed very slow filling of the retinal vessels; there was some early perfusion secondary to the cilio-retinal artery. At 7 minutes there was still significant areas of non-perfusion, as well as macular ischemia. Avastin was administered, and one week later, PRP was performed. On the day PRP was performed, the irregular iris vessels had regressed completely. She said that she had a "sliver" of vision centrally in that eye; her acuity was CF 2' and IOP 12.
Photographer: Gretchen Harper
Imaging device: Topcon
Condition/keywords: central retinal artery occlusion (CRAO), cilioretinal sparing, moyamoya, neovascularization of iris (NVI)
-
 Moyamoya: FA 7 Min OD of an Acute CRAO with CRA Sparing
Moyamoya: FA 7 Min OD of an Acute CRAO with CRA Sparing
Nov 17 2019 by John S. King, MD
60-year-old white female presented with five days of acute vision loss in the right eye. She was seen initially by referring doctor after hours five days ago and diagnosed with a CRAO and sent to ED to be evaluated stroke team. Right ICA was 100% closed but completely bypassed. She called four days later c/o redness and eye pain; at this point prominent iris vessels were seen, and she was sent to us. Her background history includes a diagnosis of Moyamoya (underwent bilateral cerebral artery bypass 2015); atorvastatin for hypercholesterolemia; ASA; no hx of HTN or Heart Disease. She had a scleral buckle repair OD in 2017 and later developed a thick ERM, which was repaired in 2018; on her previous visit her acuity was noted at 20/40. On presentation her visual acuity was HM OD and 20/15 OS. IOP was 8 OD and 10 OS. There were prominent iris vessels in the right eye, no cell or flare, and an IOL. The posterior segment exam showed diffuse retinal whitening with attenuated vessels and boxcarring; there was sparing retinal whitening in a central area of the macula that appeared to be supplied by a cilio-retina artery. The FA showed very slow filling of the retinal vessels; there was some early perfusion secondary to the cilio-retinal artery. At 7 minutes there was still significant areas of non-perfusion, as well as macular ischemia. Avastin was administered, and one week later, PRP was performed. On the day PRP was performed, the irregular iris vessels had regressed completely. She said that she had a "sliver" of vision centrally in that eye; her acuity was CF 2' and IOP 12.
Photographer: Gretchen Harper
Imaging device: Topcon
Condition/keywords: central retinal artery occlusion (CRAO), cilioretinal sparing, moyamoya, neovascularization of iris (NVI)
-
 Moyamoya: Photo OD of an Acute CRAO with CRA Sparing
Moyamoya: Photo OD of an Acute CRAO with CRA Sparing
Nov 17 2019 by John S. King, MD
60-year-old white female presented with five days of acute vision loss in the right eye. She was seen initially by referring doctor after hours five days ago and diagnosed with a CRAO and sent to ED to be evaluated stroke team. Right ICA was 100% closed but completely bypassed. She called four days later c/o redness and eye pain; at this point prominent iris vessels were seen, and she was sent to us. Her background history includes a diagnosis of moyamoya (underwent bilateral cerebral artery bypass 2015); atorvastatin for hypercholesterolemia; ASA; no hx of HTN or heart disease. She had a scleral buckle repair OD in 2017 and later developed a thick ERM, which was repaired in 2018; on her previous visit her acuity was noted at 20/40. On presentation her visual acuity was HM OD and 20/15 OS. IOP was 8 OD and 10 OS. There were prominent iris vessels in the right eye, no cell or flare, and an IOL. The posterior segment exam showed diffuse retinal whitening with attenuated vessels and boxcarring; there was sparing retinal whitening in a central area of the macula that appeared to be supplied by a cilio-retina artery. The FA showed very slow filling of the retinal vessels; there was some early perfusion secondary to the cilio-retinal artery. At 7 minutes there was still significant areas of non-perfusion, as well as macular ischemia. Avastin was administered, and one week later, PRP was performed. On the day PRP was performed, the irregular iris vessels had regressed completely. She said that she had a "sliver" of vision centrally in that eye; her acuity was CF 2' and IOP 12.
Photographer: Gretchen Harper
Imaging device: Topcon
Condition/keywords: central retinal artery occlusion (CRAO), cilioretinal sparing, moyamoya, neovascularization of iris (NVI)

 Loading…
Loading…