Search results (31 results)
-
---thumb.jpg/image-square;max$300,300.ImageHandler) Susac's Syndrome
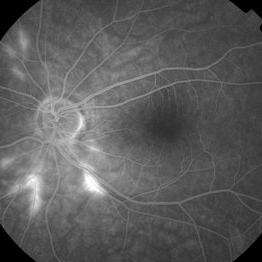
Susac's Syndrome
Oct 10 2013 by Maurice F. Rabb
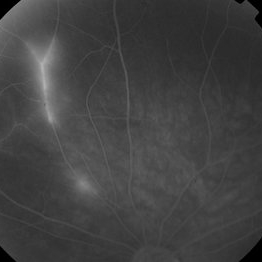
Forty one year old white male who presented for acute painless visual loss OD. There was a previous similar transient history of visual loss involving the right eye associated with a possible ill-defined cerebrovasculitis, which improved spontaneously. There also was a history of auditory difficulties. The vision at presentation was 1/200 OD, and 20/20 OS. Baseline kodachromes and a fluorescein angiogram are presented. With treatment and over a four month timeframe, the visual acuity improved to 20/25+ OD, while the left eye remained stable at 20/20.
Condition/keywords: Susac's syndrome
-
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG (FA shows a recurrence/worsening while adjusting IMT). She is stable and doing well with 20/20 vision in both eyes.
Photographer: Kay Dalby
Imaging device: Topcon
Condition/keywords: retinal vasculitis, Susac's syndrome
-
28-Year-Old Male With Susac's Syndrome
Feb 2 2015 by Gregory J. Mincey, MD, MBA
Recurrent proliferative disease after initial stabilization with PRP.
Photographer: Bill McVerry, Carolina Eye Associates
Imaging device: Topcon
Condition/keywords: Susac's syndrome
-
Neovascularization and Ischemia Susac's Syndrome
Feb 2 2015 by Gregory J. Mincey, MD, MBA
28-year-old man with bilateral Susac's with ischemia and neovascularization.
Photographer: Bill McVerry, Carolina Eye Associates
Condition/keywords: Susac's syndrome
-
Persistent Neovascularization in 28-Year-Old Male With Susac's
Feb 2 2015 by Gregory J. Mincey, MD, MBA
Persistent proliferative disease after second PRP in 28-year-old with Susac's.
Photographer: Bill McVerry, Carolina Eye Associates
Imaging device: Topcon TRC50DX
Condition/keywords: Susac's syndrome
-
Proliferative Disease in Susac's
Feb 2 2015 by Gregory J. Mincey, MD, MBA
Recurrent proliferative disease after initial stabilization with PRP.
Photographer: Bill McVerry, Carolina Eye Associates
Imaging device: Topcon TRC50DX
Condition/keywords: Susac's syndrome
-
Susac's Syndrome
Feb 2 2015 by Gregory J. Mincey, MD, MBA
Peripheral ischemia and neovascularization.
Photographer: Bill McVerry, Carolina Eye Associates
Imaging device: Topcon TRC50DX
Condition/keywords: Susac's syndrome
-
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
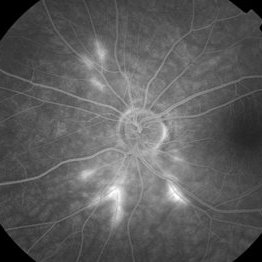
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO superotemporally OD (see photo), and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathioprine, and MTX, and has had the best reponse to IVIG. She is stable and doing well with 20/20 vision in both eyes.
Photographer: Macey Highfill
Imaging device: Topcon
Condition/keywords: Susac's syndrome
-
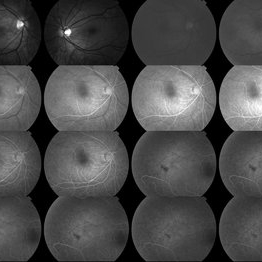 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO superitemporally OD, and bilateral arteritis (see initial FA). She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathioprine, and MTX, and has had the best reponse to IVIG. She is stable and doing well with 20/20 vision in both eyes.
Photographer: Maycey Highfill
Imaging device: Topcon
Condition/keywords: Susac's syndrome
-
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and superotemporal BRAO OD, and bilateral arteritis (initial FAs). She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathioprine, and MTX, and has had the best reponse to IVIG. She is stable and doing well with 20/20 vision in both eyes.
Photographer: Maycey Highfill
Imaging device: Topcon
Condition/keywords: Susac's syndrome
-
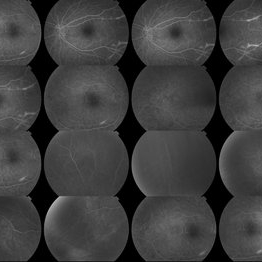
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG. She is stable and doing well with 20/20 vision in both eyes (most recent FA)
Photographer: Kay Dalby
Imaging device: Topcon
Condition/keywords: retinal vasculitis, Susac's syndrome
-
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG Background: 46yo WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG (FA shows a recurrence/worsening while adjusting IMT). She is stable and doing well with 20/20 vision in both eyes.
Photographer: Kay Dalby
Imaging device: Topcon
Condition/keywords: retinal vasculitis, Susac's syndrome
-
---thumb.jpg/image-square;max$300,300.ImageHandler) Susac's Syndrome
Susac's Syndrome
Oct 10 2013 by Maurice F. Rabb
Forty one year old white male who presented for acute painless visual loss OD. There was a previous similar transient history of visual loss involving the right eye associated with a possible ill-defined cerebrovasculitis, which improved spontaneously. There also was a history of auditory difficulties. The vision at presentation was 1/200 OD, and 20/20 OS. Baseline kodachromes and a fluorescein angiogram are presented. With treatment and over a four month timeframe, the visual acuity improved to 20/25+ OD, while the left eye remained stable at 20/20.
Condition/keywords: Susac's syndrome
-
---thumb.jpg/image-square;max$300,300.ImageHandler) Susac's Syndrome
Susac's Syndrome
Oct 10 2013 by Maurice F. Rabb
Forty one year old white male who presented for acute painless visual loss OD. There was a previous similar transient history of visual loss involving the right eye associated with a possible ill-defined cerebrovasculitis, which improved spontaneously. There also was a history of auditory difficulties. The vision at presentation was 1/200 OD, and 20/20 OS. Baseline kodachromes and a fluorescein angiogram are presented. With treatment and over a four month timeframe, the visual acuity improved to 20/25+ OD, while the left eye remained stable at 20/20.
Condition/keywords: Susac's syndrome
-
---thumb.jpg/image-square;max$300,300.ImageHandler) Susac's Syndrome
Susac's Syndrome
Oct 10 2013 by Maurice F. Rabb
Forty one year old white male who presented for acute painless visual loss OD. There was a previous similar transient history of visual loss involving the right eye associated with a possible ill-defined cerebrovasculitis, which improved spontaneously. There also was a history of auditory difficulties. The vision at presentation was 1/200 OD, and 20/20 OS. Baseline kodachromes and a fluorescein angiogram are presented. With treatment and over a four month timeframe, the visual acuity improved to 20/25+ OD, while the left eye remained stable at 20/20.
Condition/keywords: Susac's syndrome
-
---thumb.jpg/image-square;max$300,300.ImageHandler) Susac's Syndrome
Susac's Syndrome
Oct 10 2013 by Maurice F. Rabb
Forty one year old white male who presented for acute painless visual loss OD. There was a previous similar transient history of visual loss involving the right eye associated with a possible ill-defined cerebrovasculitis, which improved spontaneously. There also was a history of auditory difficulties. The vision at presentation was 1/200 OD, and 20/20 OS. Baseline kodachromes and a fluorescein angiogram are presented. With treatment and over a four month timeframe, the visual acuity improved to 20/25+ OD, while the left eye remained stable at 20/20.
Condition/keywords: Susac's syndrome
-
---thumb.jpg/image-square;max$300,300.ImageHandler) Susac's Syndrome
Susac's Syndrome
Oct 10 2013 by Maurice F. Rabb
Forty one year old white male who presented for acute painless visual loss OD. There was a previous similar transient history of visual loss involving the right eye associated with a possible ill-defined cerebrovasculitis, which improved spontaneously. There also was a history of auditory difficulties. The vision at presentation was 1/200 OD, and 20/20 OS. Baseline kodachromes and a fluorescein angiogram are presented. With treatment and over a four month timeframe, the visual acuity improved to 20/25+ OD, while the left eye remained stable at 20/20.
Condition/keywords: Susac's syndrome
-
---thumb.jpg/image-square;max$300,300.ImageHandler) Susac's Syndrome
Susac's Syndrome
Oct 10 2013 by Maurice F. Rabb
Forty one year old white male who presented for acute painless visual loss OD. There was a previous similar transient history of visual loss involving the right eye associated with a possible ill-defined cerebrovasculitis, which improved spontaneously. There also was a history of auditory difficulties. The vision at presentation was 1/200 OD, and 20/20 OS. Baseline kodachromes and a fluorescein angiogram are presented. With treatment and over a four month timeframe, the visual acuity improved to 20/25+ OD, while the left eye remained stable at 20/20.
Condition/keywords: Susac's syndrome
-
---thumb.jpg/image-square;max$300,300.ImageHandler) Susac's Syndrome
Susac's Syndrome
Oct 10 2013 by Maurice F. Rabb
Forty one year old white male who presented for acute painless visual loss OD. There was a previous similar transient history of visual loss involving the right eye associated with a possible ill-defined cerebrovasculitis, which improved spontaneously. There also was a history of auditory difficulties. The vision at presentation was 1/200 OD, and 20/20 OS. Baseline kodachromes and a fluorescein angiogram are presented. With treatment and over a four month timeframe, the visual acuity improved to 20/25+ OD, while the left eye remained stable at 20/20.
Condition/keywords: Susac's syndrome
-
---thumb.jpg/image-square;max$300,300.ImageHandler) Susac's Syndrome
Susac's Syndrome
Oct 10 2013 by Maurice F. Rabb
Forty one year old white male who presented for acute painless visual loss OD. There was a previous similar transient history of visual loss involving the right eye associated with a possible ill-defined cerebrovasculitis, which improved spontaneously. There also was a history of auditory difficulties. The vision at presentation was 1/200 OD, and 20/20 OS. Baseline kodachromes and a fluorescein angiogram are presented. With treatment and over a four month timeframe, the visual acuity improved to 20/25+ OD, while the left eye remained stable at 20/20.
Condition/keywords: Susac's syndrome
-
 Susac's syndrome
Susac's syndrome
Dec 5 2017 by Marina Gilca, MD
Fluorescein angiogram of a 33 year-old female presenting with recurrent scotomas OS.
Photographer: Retina Consultants LTD
Condition/keywords: scotoma
-
 Susac's syndrome
Susac's syndrome
Dec 5 2017 by Marina Gilca, MD
Fluorescein angiogram of the right eye of a 33-year-old female presenting with recurrent scotomas OS.
Photographer: Retina Consultants LTD
Condition/keywords: Susac's syndrome
-
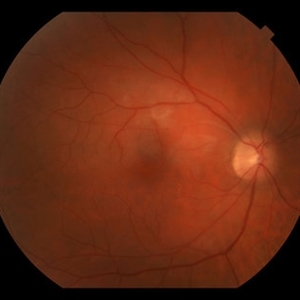
Susac's Syndrome
Sep 4 2017 by Amir Manor, MD
Fundus photograph of a 19-year-old man with Susac's syndrome.
Photographer: Galit Yair Pur
Condition/keywords: color fundus photograph, Susac's syndrome
-
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG (FA shows a recurrence/worsening while adjusting IMT). She is stable and doing well with 20/20 vision in both eyes.
Photographer: Kay Dalby
Imaging device: Topcon
Condition/keywords: retinal vasculitis, Susac's syndrome
-
 Susac's Syndrome
Susac's Syndrome
Feb 13 2018 by John S. King, MD
Background: 46-year-old WF with CML (stable on Sprycel) saw her PCP for headaches without known cause; Headaches worsened and became confused, disoriented, off balance, and impaired short term memory. Heme-oncology ordered MRI that showed abnormal signal in the cerebellum and other parts of the brain, and LP has elevated protein. LP did show positive tau test, but fortunately, was a false positive for CJD. IV and PO steroids started and symptoms improved. MRI showed much improvement one month since starting steroids. 3 weeks later had a scotoma in right eye and eye doctor did not find anything at that time to cause it. Tinnitus developed (and some intermittent vertigo before that) and ENT referred back to eye doctor, who then referred the patient to Dr. Zocchi. He found a CWS and BRAO OD, and bilateral arteritis. She had some additional work-up for vasculitis. Given the retinal arteritis, cochlear issues, and MRI findings, Dr.Zocchi suspected Susac's Syndrome. She was started on multiple regimens including prednisone, IVIG, azathiprine, and MTX, and has had the best reponse to IVIG (FA shows a recurrence/worsening while adjusting IMT). She is stable and doing well with 20/20 vision in both eyes.
Photographer: Macey Highfill
Imaging device: Topcon
Condition/keywords: retinal vasculitis, Susac's syndrome

 Loading…
Loading…