-
 Central Retinal Artery Occlusion Leading to Patent Foramen Ovale Diagnosis
Central Retinal Artery Occlusion Leading to Patent Foramen Ovale Diagnosis
Sep 13 2019 by Patrícia José Figueiredo Lopes
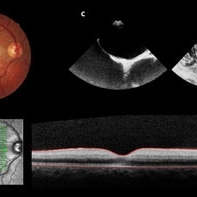
A 19-year-old man presented in emergency department (ED) reporting painless blurred vision in the right eye that started one hour ago while he was doing exercise. His medical history was unremarkable. On examination, best corrected visual acuity in the right eye was counting fingers (20cm), right relative afferent pupillary defect was evident, intraocular pressure and anterior segment were normal. Dilated retinal examination revealed retinal whitening in the macular area and a cherry red spot (panel A) that became increasingly evident with time. Patient denied other systemic symptoms. Macular spectral domain optic coherence tomography showed hyperreflectivity of the inner retina (panel B). In ED, patient underwent ocular massage using a three-mirror contact lens and topical hypotensive treatment. Additionally, oral antiplatelet and hyperbaric oxygen treatment were initiated. Further investigation was performed and fluorescein angiography revealed a delay in arterial filling. Blood tests including hypercoagulation disorders investigation, plain chest radiography and electrocardiogram were unremarkable. Patent foramen ovale was diagnosed in transesophageal echocardiogram (panel C), anticoagulation therapy was promptly initiated and percutaneous closure of patent foramen ovale was done successfully a few weeks later. Final best corrected visual acuity was 20/200 and macula developed atrophy.
Photographer: Patrícia José
Condition/keywords: central retinal artery occlusion (CRAO), patent foramen ovale
-
 Lipemia Retinalis: Key to Diagnose a Systemic Disease
Lipemia Retinalis: Key to Diagnose a Systemic Disease
Aug 6 2020 by Patrícia José Figueiredo Lopes
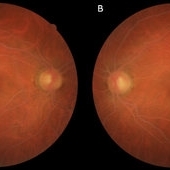
A 49-year-old female with history of insulin-dependent diabetes mellitus, hypertension and hyperlipidemia (managed with HMG-CoA reductase inhibitor plus lipid-lowering compound that inhibits intestinal cholesterol and phytosterol absorption) presented in a routine ophthalmology appointment. On examination, best-corrected visual acuity was 20/20 with an unremarkable anterior segment bilaterally. Funduscopic examination showed no signs of diabetic retinopathy. However, retinal vessels were creamish milky white, only distinguished by their size, suggesting lipemia retinalis (A, right eye; B, left eye). Triglyceride levels were 1500 mg/dL (normal range 0-150 mg/dL). Lipemia retinalis is a rare manifestation of hyperlipidemia but is a valuable tool for the diagnosis and treatment of this disease. The characteristic funduscopic findings include retinal blood vessels discoloration ranging from salmon pink to creamish white, depending on the level of plasma triglycerides. There are few reports about retinal changes in hypertriglyceridemia and all disclose triglyceride concentration exceeding 2,500 mg/dl.
Condition/keywords: hyperlipidemia, lipemia retinalis
-
 Choroidal Vessels
Choroidal Vessels
Oct 28 2021 by Patrícia José Figueiredo Lopes
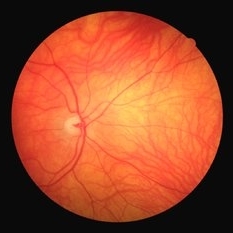
A 30-year-old male with a positive history of HIV was referred to ophthalmology department to rule out retinal lesions. On examination, best-corrected visual acuity was 20/20 with an unremarkable anterior segment bilaterally. Funduscopic examination showed no signs of HIV retinopathy. However, his choroidal vessels were really impressive.
Photographer: Patrícia José, Serviço de Oftalmologia, Hospital Santa Maria, Centro Hospitalar Universitário Lisboa Norte, Portugal
Condition/keywords: choroidal vessels

A project from the American Society of Retina Specialists