-
 By JEFFERSON R SOUSA, Tecg.º (Biomedical Systems Technology)
By JEFFERSON R SOUSA, Tecg.º (Biomedical Systems Technology)
Lens Oftalmologia - Hospital Beneficiência Portuguesa - Uploaded on May 9, 2023.
- Last modified by Joshua Friedman on May 9, 2023.
- Rating
- Appears in
- Miscellaneous
- Condition/keywords
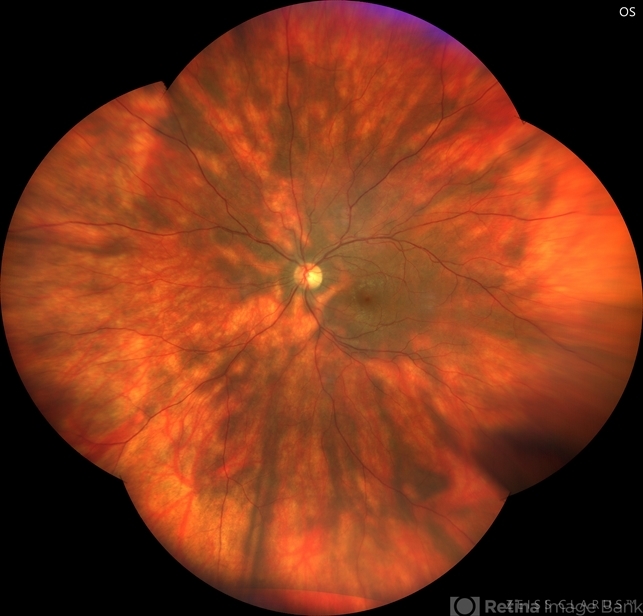
- birdshot, birdshot chorioretinopathy, birdshot retinochoroidopathy, bilateral chorioretinal folds, birdshot choroidopathy
- Photographer
- JEFFERSON ROCHA DE SOUSA - Retinal Department at Institute Dr. Suel Abujamra Sao Paulo-Brazil
- Imaging device
-
Fundus camera
Clarus 700 - Zeiss, composite of four 135 degree images. - Description
- Female patient, 41 years old, with progressive low visual acuity, progressive history of autoimmune disease. In the multimodal retinal fundoscopic evaluation, important characteristics compatible with "Birdshot Retinopathy" were observed. Birdshot retinopathy, also known as birdshot chorioretinopathy or birdshot uveitis, is a rare, chronic inflammatory disorder that affects the retina and the choroid of the eye. It typically develops in adults between the ages of 30 and 60 years, and is more common in women than men. The name "birdshot" refers to the small, round, yellow-white spots that appear on the retina, which resemble the pattern of a shotgun blast. These spots are caused by inflammation in the eye, and can lead to vision loss if left untreated. Symptoms of birdshot retinopathy include blurred vision, floaters, loss of night vision, and difficulty adapting to changes in lighting. The condition can also cause inflammation in other parts of the eye, leading to redness, pain, and sensitivity to light. The exact cause of birdshot retinopathy is unknown, but it is believed to be an autoimmune disorder, in which the body's immune system mistakenly attacks the retina and choroid. Treatment typically involves the use of immunosuppressive medications, such as corticosteroids or biologic agents, to reduce inflammation and preserve vision. Close monitoring by an ophthalmologist is important, as the disease can progress even with.

 Initializing download.
Initializing download.





---thumb.jpg/image-square;max$79,0.ImageHandler)