44 yo WF seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), Plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU......... Va 20/200 OD and 20/20 OS, IOP 12 OU, Pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery. There was trace vitreous cell OS, mild disc edema, and a large, granular placoid area nasally that appeared to be granulated. The OCT showed mild subfoveal fluid with nodular areas in the RPE and some overlying irregular architecture of the outer retina.......Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand, and later learned that she had a rash on the soles of her feet..... She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started).... She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated. OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer.
-
 Posterior Placoid Chorioretinopathy
Posterior Placoid Chorioretinopathy
Dec 19 2020 by John S. King, MD
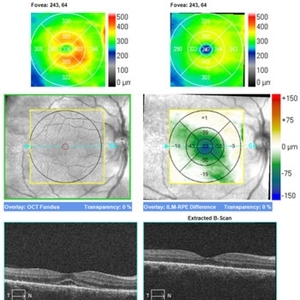
44-year-old white female seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU. Va 20/200 OD and 20/20 OS, IOP 12 OU, Pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery. There was trace vitreous cell OS, mild disc edema, and a large, granular placoid area nasally that appeared to be granulated. The OCT showed mild subfoveal fluid with nodular areas in the RPE and some overlying irregular architecture of the outer retina. Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand, and later learned that she had a rash on the soles of her feet. She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started). She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated. OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer (See Image).
Imaging device: Zeiss Cirrus
Condition/keywords: acute syphilitic posterior placoid chorioretinitis, syphilis
-
 Posterior Placoid Chorioretinopathy
Posterior Placoid Chorioretinopathy
Dec 19 2020 by John S. King, MD
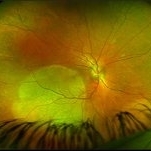
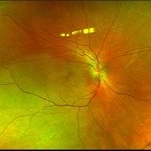
44-year-old white female seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), Plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU. Va 20/200 OD and 20/20 OS, IOP 12 OU, pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery, and two possible smaller spots SN (See Photo above). There was a trace vitreous cell OS with a large, granular placoid lesion nasally. The OCT showed mild subfoveal fluid with nodular areas in the RPE and some overlying irregular architecture of the outer retina. Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand, and later learned that she had a rash on the soles of her feet. She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started). She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated. OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer.
Imaging device: Optos CA
Condition/keywords: acute syphilitic posterior placoid chorioretinitis, syphilis
-
 Syphilis Placoid Initial Image OS
Syphilis Placoid Initial Image OS
Dec 19 2020 by John S. King, MD
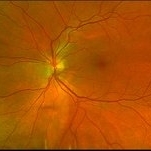
44-year-old white female seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU. Va 20/200 OD and 20/20 OS, IOP 12 OU, pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery. There was trace vitreous cell OS, mild disc edema, and a large, granular placoid area nasally that appeared to be granulated (See Image). The OCT showed mild subfoveal fluid with nodular areas in the RPE and some overlying irregular architecture of the outer retina. Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand, and later learned that she had a rash on the soles of her feet. She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started).... She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated. OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer.
Imaging device: Optos CA
Condition/keywords: acute syphilitic posterior placoid chorioretinitis, syphilis
-
 Posterior Placoid Chorioretinopathy
Posterior Placoid Chorioretinopathy
Dec 19 2020 by John S. King, MD
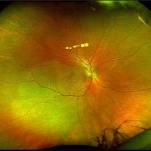
44-year-old white female seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU. Va 20/200 OD and 20/20 OS, IOP 12 OU, pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery. There was trace vitreous cell OS, mild disc edema, and a large, granular placoid area nasally that appeared to be granulated. The OCT showed mild subfoveal fluid with nodular areas in the RPE and some overlying irregular architecture of the outer retina. Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand, and later learned that she had a rash on the soles of her feet. She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started). She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated (See Image). OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer.
Photographer: Ashley Seiger
Imaging device: Optos CA
Condition/keywords: acute syphilitic posterior placoid chorioretinitis, syphilis
-
 Posterior Placoid Chorioretinopathy
Posterior Placoid Chorioretinopathy
Dec 19 2020 by John S. King, MD
44-year-old white female seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU. Va 20/200 OD and 20/20 OS, IOP 12 OU, pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery. There was trace vitreous cell OS, mild disc edema, and a large, granular placoid area nasally that appeared to be granulated. The OCT showed mild subfoveal fluid with nodular areas in the RPE and some overlying irregular architecture of the outer retina. Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand, and later learned that she had a rash on the soles of her feet. She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started). She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated (See Image). OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer.
Photographer: Ashley Seiger
Imaging device: Optos CA
Condition/keywords: acute syphilitic posterior placoid chorioretinitis
-
 Posterior Placoid Chorioretinopathy
Posterior Placoid Chorioretinopathy
Dec 19 2020 by John S. King, MD
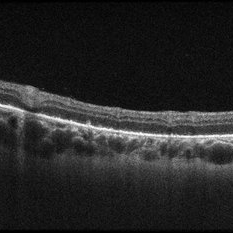
44-year-old white female seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU. Va 20/200 OD and 20/20 OS, IOP 12 OU, pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery. There was a trace vitreous cell OS with a large, granular placoid lesion nasally. The OCT via the lesion (see above) shows nodular areas in the RPE and some overlying disruption of EZ and outer retina. Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand, and later learned that she had a rash on the soles of her feet. She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started). She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated. OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer.
Imaging device: Zeiss Cirrus
Condition/keywords: acute syphilitic posterior placoid chorioretinitis, syphilis
-
 Posterior Placoid Chorioretinopathy
Posterior Placoid Chorioretinopathy
Dec 19 2020 by John S. King, MD
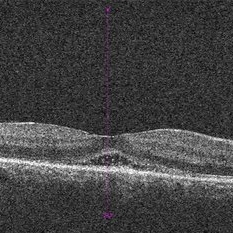
44-year-old white female seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU. Va 20/200 OD and 20/20 OS, IOP 12 OU, pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery. There was a trace vitreous cell OS with a large, granular placoid lesion nasally. The OCT (see above) shows mild subfoveal fluid with nodular areas in the RPE and some overlying irregular architecture of the outer retina. Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand, and later learned that she had a rash on the soles of her feet. She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started). She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated. OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer.
Imaging device: Zeiss Cirrus
Condition/keywords: acute syphilitic posterior placoid chorioretinitis, syphilis
-
 Palms of Patient with Placoid Lesions in Posterior Segment
Palms of Patient with Placoid Lesions in Posterior Segment
Dec 20 2020 by John S. King, MD
44-year-old white female seen over the weekend complaining of a "spot" in her vision centrally OD for three days. She was referred over by another eye doctor who was concerned about a possible retinal detachment vs ARN in that eye. Her past medical history includes adrenal insufficiency for which she takes a low dose of hydrocortisone, thyroxine (post thyroidectomy), Plaquenil (inflammatory arthritis). She is divorced with one partner and denies any IVDU. Va 20/200 OD and 20/20 OS, IOP 12 OU, Pupils mydriatic post gtts (light desaturation OD). There was 1+ A/C cell OD, O/W unremarkable anterior segment OU; in the posterior segment OD there was 1+ vitritis with a diffusely swollen optic disc and a large yellowish placoid lesion in the macula with yellowish border and extended out past the arcades inferiorly, as well as another lesion smaller in the IN periphery. There was trace vitreous cell OS, mild disc edema, and a large, granular placoid area nasally that appeared to be granulated. The OCT showed mild subfoveal fluid with nodular areas in the RPE and some overlying irregular architecture of the outer retina. Syphilis was a concern at this point. She denied any hand or foot rash, and said that she was recently working on the house, and her hands were dried out. There did appear to be a rash on the hand (See Image), and later learned that she had a rash on the soles of her feet. She was sent to ED for a work-up and her syphilis IgG was positive and VDRL 1:128, and negative for HIV. She was started on a course IV Penicillin (40mg PO steroid two days after tx started). She has responded well. A few days after treatment her visual acuity has improved to 20/60 OD; there was no anterior segment inflammation OU, and decreased vitreous cell OU. Disc edema was improved. The large placoid lesion in the macula of the right eye was slightly enlarged, but more granular in appearance without a distinct yellowish border, and the smaller lesions SN had dissipated. OCT showed resolution of the subfoveal fluid and an improved appearance of the outer retina and RPE layer.
Imaging device: Optos CA
Condition/keywords: acute syphilitic posterior placoid chorioretinitis
